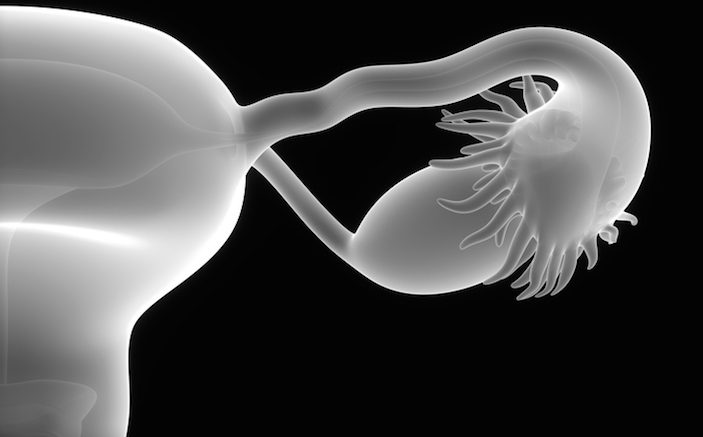
Diagnosing ovarian torsion in the emergency department remains a challenge. Any female patient who presents with abdominal pain should prompt consideration of torsion in ED providers. While the overall incidence of ovarian torsion is low and there is almost no associated mortality, when missed, ovarian torsion can result in a significant degree of morbidity for the patient and medicolegal risk for the provider. To minimize the risk of missing a case of ovarian torsion, we’ll cover several important pitfalls and misconceptions related to the workup of potential torsion. In this month’s issue we’ll discuss history and exam – and part two will cover imaging and disposition.
The Risk to the Patient May Be Overstated
It is hard to quantify the exact risk to the patient in cases of missed ovarian torsion. There are no known reports of increased mortality in cases of missed torsion. In terms of morbidity, reduced fertility is commonly cited as an outcome in cases of torsion that result in the loss of an ovary; however, the evidence to support this claim is limited. Animal studies have reported similar fertility rates both before and after the removal of an ovary [1]. Bellati et al. found that patients who had one ovary surgically removed were able to become pregnant at rates similar to those seen in patients who underwent non-gyenocologic abdominal procedures [2].
The Risk to the Provider Is Real
Despite the weak scientific evidence connecting loss of an ovary to decreased fertility, this potential outcome is mentioned as a potential damage in multiple legal cases involving cases of missed ovarian torsion. Most cases of missed torsion involve either a failure to consider the diagnosis initially or cases of intermittent torsion. Given the medicolegal risk associated with cases of missed torsion, providers should consider and document the possibility of torsion in any patient with undifferentiated abdominal pain.
Classic Findings Are Not Reliable
Making the diagnosis of ovarian torsion in the ED can be difficult as patients across a wide range of demographics can present with variable and atypical symptoms. Pain from ovarian torsion has classically pain been described as sharp, sudden, and unilateral; however, in practice these historical features can not be used to reliably rule out cases of torsion. In a retrospective review of 87 cases of torsion, Houry et al. found that 70% of patients reported “sharp or stabbing” pain. Symptoms started abruptly in 59% of cases, and 70% of patients reported associated nausea and vomiting.
Historical features such as the patients age and medical history are similarly unreliable. While the majority of cases of torsion occur in women of reproductive age, up to 15% of cases occur in the pediatric population with a similar percentage of cases occurring in patients who are post-menopausal. In addition up to 20% of cases may occur during pregnancy. While most patients with torsion will have a structurally abnormal ovary, only 25% of patients will report previous history of ovarian cyst or mass.
Do not rely on the physical exam Bedside exam is rarely helpful when trying to make the diagnosis of ovarian torsion. Torsion can present with a wide variety of symptoms, with up to 30% of patients reporting no abdominal pain. While abnormal exam findings may increase a provider’s level of concern, the bedside exam suffers from poor sensitivity and specificity and can not be used to rule out cases of torsion. The pelvic exam has similar limitations, and has not been shown to reliably identify abnormal ovarian or adnexal findings. Even in what would seem like near ideal conditions, attending gynecologists performing pelvic exams in an operative setting reported sensitivities ranging from 15-36% when trying to detect adnexal masses. In cases of potential torsion, abnormal exam findings may help make the diagnosis; but a normal exam does not adequately decrease the likelihood of the disease.
Beware Intermittent Torsion
Cases of intermittent ovarian torsion pose a significant diagnostic challenge. Clinically, patients may experience dynamic torsing and detorsing of the ovary leading to intermittent symptoms and variable radiographic findings. To date there is limited evidence that can help reliably identify cases of intermittent ovarian torsion. Despite an overall low incidence of cases of intermittent torsion, providers should consider the diagnosis when patients have continued symptoms.
Given the significant medicolegal risk associated with cases of missed torsion, providers need to consider and document the potential risk of intermittent torsion in any patient with unexplained abdominal pain. If the concern for ongoing torsion is high (such as in a patient with sudden onset sharp pain, or known ovarian cysts), it would be reasonable to consult OB/GYN. In cases with a lower concern for torsion, providers should give clear verbal and written discharge instructions and return precautions.
In Part II we will look at the pitfalls and misconceptions associated with the diagnostic approach to cases of potential ovarian torsion.
REFERENCES
- Mohan M, Rajamahendran R. Effects of unilateral ovariectomy on follicular development and ovulation in cattle. Theriogenology. 1998 Apr 1;49(5):1059-70. PubMed PMID: 10732113.
- Bellati F, Ruscito I, Gasparri ML, Antonilli M, Pernice M, Vallone C, Morano G, Chirletti P, Berloco PB, Panici PB. Effects of unilateral ovariectomy on female fertility outcome. Arch Gynecol Obstet. 2014 Aug;290(2):349-53. doi: 10.1007/s00404-014-3194-8. Epub 2014 Mar 11. PubMed PMID: 24615568
- Houry D, Abbott JT. Ovarian torsion: a fifteen-year review. Ann Emerg Med. 2001 Aug;38(2):156-9. PubMed PMID: 11468611.
- Schmitt ER, Ngai SS, Gausche-Hill M, Renslo R. Twist and shout! Pediatric ovarian torsion clinical update and case discussion. Pediatr Emerg Care. 2013 Apr;29(4):518-23; quiz 524-6. doi: 10.1097/PEC.0b013e31828a7822. Review. PubMed PMID: 23558274.
- Padilla LA, Radosevich DM, Milad MP. Accuracy of the pelvic examination in detecting adnexal masses. Obstet Gynecol. 2000 Oct;96(4):593-8. PubMed PMID: 11004365.