The challenges of treating the ill and injured at a 30,000 person festival.
When staffing music festivals, be prepared to treat an interesting mix of pathology. While much of the pathology is predictable based on the specific type of festival and a historical analysis of the previous medical care provided, patient presentations are quite variable between different types of music festivals featuring different music and mood.
Crowd mood, a term frequently discussed in the mass gathering medicine literature, is an important descriptor to determine crowd behavior and should be utilized as a tool to predict the patient presentation rate (PPR). Other major factors contributing to the PPR and the transport to hospital rate (TTHR) are the heat index and the amount and type of recreational drug use. For every ten-degree increase in the heat index, the medical team can anticipate three more patients per 10,000 attendees.
Some festivals have stringent security procedures utilizing canine units at venue entrances and undercover law enforcement actively looking to arrest drug sellers while other festivals have relatively lax security measures. As emergency physicians, we always prepare for the worst and we recommend multiple resuscitation areas set up for rapid sequence intubations as well as premade ice-baths and unobstructed egress off the site for critical patients.
Severely hyperthermic patients present to on-site medical teams frequently and we should be prepared to treat significant rhabdomyolysis causing acute renal failure, which in turn can cause critical hyperkalemia and acidemia. Below are some interesting cases and lessons learned from the festival which included a range of pathology such as toxicological emergencies, status epilepticus, orthopedic injuries, major trauma, crotalid envenomations, and Point Of Care Ultrasound for the win!
CASE 1:
Day 1 started off with our first patient, a male in his early 20s who decided to grab a baby RATTLESNAKE, sustaining a bite to his index finger.
After some south Brooklyn-based EM physicians conferred together, we noted that the basic workup of CBC, chemistry, coagulation profile, and fibrinogen were not feasible in the field. Additionally, it is important to note that it is believed that younger snakes have less control of their envenomations, so these bites are considered more risky, despite appearing benign! It is unclear how many of these bites are “dry bites” however one educational source suggested that “dry bites” occur in approximately 25% of Crotalinae snake bites in the U.S. and therefore show only minimal local irritation.
Polyvalent Crotalinae ovine immune Fab (FabAB, Crofab, Psotherics) is indicated when there is rapid progression of swelling, abnormal labs (platelets<100,000 or fibrinogen <100), or there are systemic manifestations (AMS or unstable VS). The initial dose is 4-6 vials, and this may need to be repeated if symptoms are not controlled. Given this patient’s minimal physical exam findings after a period of observation, we decided to continue observing for progression of swelling and erythema and the patient returned for regular wound checks over the next 12 hours.

At the 12-hour mark, there were mild local findings around the bite, but no evidence of progression up the hand, and the patient was discharged with wound-care/follow-up instructions and return precautions.
Perhaps the most important lesson: when working outside of your normal comfort zone, you must know what your local resources can offer and which medical facilities offer specific capabilities. Options for transporting critical patients to definitive care facilities should be prearranged. Many ground ALS ambulances do not feel comfortable transporting ventilated and paralyzed patients for extended transports thus more rapid transport by aeromedical rotor or fixed-wing options should be initiated promptly without increasing delays.
In the case of our first patient, the closest hospital thought they had CroFab but when asked a second time they actually did not. Thus, the medical team would need to confirm antivenin in stock prior to transporting a patient to a specific facility and determine the best transport option if there are real systemic manifestations.
Teaching Points:
DO: immobilize the limb in a neutral position, remove jewelry, mark edges of erythema/edema
DO NOT: attempt to suck out venom, place affected part in cold water, use tourniquet or wrap
**ANTIVENIN(CroFab) is the treatment for compartment syndrome; fasciotomy is a last resort**
- True envenomation produces swelling, pain, ecchymoses, and blistering; proximal spread suggests progressive toxicity.
- Systemic reactions (i.e., nausea, vomiting, abdominal pain, paresthesias, dizziness) suggest more severe envenomations; hypotension and AMS are ominous findings, and these patients require emergent antivenin.
- Determine closest access to antivenin (1st dose = 4-6 vials) and best mode of transportation for emergent treatment. Some hospitals only carry the first dose; Patients with systemic reactions could be sent to closer hospitals for the initial dose and then transported from there for further doses/treatment.
CASE 2:
There were multiple cases of patients presenting with SVT, one after smuggled recreational substances placed in zip lock bags in a patient’s vagina leaked out of the bags. That patient was successfully chemically cardioverted with adenosine. Another patient presented with SVT and the modified Valsalva maneuver based on the REVERT trial was performed with success!
Teaching Points:
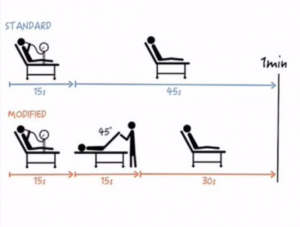
Modified Positional Valsalva for stable SVT: goal is to induce a vagal reflex by having patient increase intrathoracic pressure with Valsalva and give them a bolus of venous return by raising legs.
Set-up: 10cc syringe with plunger (loosen plunger), two assistants – one to adjust HOB and another to raise/lower legs, keep patient on monitor
- Position patient with legs flat and HOB at 45°
- Have patient attempt to blow out plunger of 10cc syringe (or Valsalva around 40mmHg) for 15s
- Quickly reposition patient’s head of bed to the supine position and raise legs to 45° for 15s
- Return to original position and continue to monitor for 1 min
- Repeat if needed
– If using adenosine, some literature supports a 3rd dose of 18mg if 12mg fails.
– Consider initial adult dose of 3mg of adenosine if: central line (decreased transit time to myocardium), heart transplant (relative sensitivity of denervated transplanted hearts), patient on carbamazepine or dipyridamole
CASE 3:
A young male presented holding his left upper quadrant after a self-inflicted stab wound. It was quickly determined that the patient had a left sucking chest wound. The patient was pale and diaphoretic although his vital signs were stable. A FAST was performed which was negative. A small-bore chest tube was placed and the patient was transported by a rotor wing aircraft to the nearest trauma center with greater than 700cc output of blood from the chest tube. At the trauma center, the patient was found to have a persistent hemothorax and pneumothorax and was taken to the OR for exploration. No definitive injury was identified and the patient was doing well a couple of days later.

Teaching Points:
– Occlusive dressing over puncture wounds – chest seals with one-way valves ensure unidirectional air flow preventing a pneumothorax from expanding or converting to a tension pneumothorax
– Hemostatic agents for actively bleeding penetrating wounds work by several different mechanisms such as exerting physical, tamponading effects or by enhancing hemostatic mechanisms. External agents such as QuickClot are soaked with an inorganic product (kaolin) which activates factor XII to start the coagulation cascade. The HemCon bandage is composed of chitosan, a biodegradable complex carbohydrate, which tamponades and seals bleeding vessels. Biologically active agents augment hemostasis by combining topical thrombin with gelatinous foam or granules.
– Flight physiology – As altitude increases, pressure decreases and as per Boyle’s law, volume increases. Every pneumothorax needs to be decompressed before flying otherwise there is a concern for converting that pneumothorax into a tension pneumothorax. Effects are compounded by positive pressure ventilation so it is better to avoid intubating the patient if at all possible. A patient with a pneumothorax who needs intubation would need to have the chest decompressed prior to flying. Another indication for decompression is if the patient cannot be observed closely during the flight due to confined space or multiple patients.
– Perhaps a larger bore chest tube would have been preferable, but in austere medicine, we have to make do with limited resources.
– Can consider clearing patients to fly commercially two weeks after full resolution of traumatic pneumothorax.
CASE 4:
There was a 21 year-old male who was intoxicated after ingesting psychostimulants and presented with altered mental status (AMS) and severe agitation. The patient was chemically sedated with IM ketamine. The patient was then promptly found to have a core temperature of 108.7. The patient was immediately dunked in a premade ice bath for approximately 8.5 minutes with cold IV fluids running with multiple peripheral large bore access options. The patient was given dantrolene, paralyzed and intubated, electrolytes checked, and the core temperature was reduced to 100.3. The patient was in the air 35 minutes after the initial temperature was obtained. The patient was extubated the next day neurologically intact and transferred from the ICU to the medical floor.
Teaching Points:
– Hyperthermia secondary to psychostimulant drug induced toxicity (PDIT)– must obtain prompt core temperatures on all AMS patients. This is a tough feat because many patients present with AMS, however the importance cannot be overstated to determine who needs emergent, intensive treatment to prevent multisystem end-organ damage.
– Prioritize chemical sedation with ketamine or benzodiazepines. Consider neuroleptics if other agents are not available. Olanzapine is preferred over Haldol as it’s approximately twice as potent and safer in patients with prolonged QT intervals.
– Management: Ice water immersion, infuse cold fluids through every body cavity, RSI for muscle contraction cessation, increase respiratory rate once intubated as patients are acidotic. Must monitor electrolyte abnormalities (think ARF and hyperkalemia). There isn’t much data supporting dantrolene for psychostimulant drug induced toxicity and the reported data suffers from publication bias and selection bias. However, anecdotally dantrolene seems to quickly reduce core temperature. Core temperatures of patients submerged in ice water baths drops approximately 3°F for every five minutes in the bath. Aim for a temperature of 101°F to prevent overshooting. Mitigate shivering with fentanyl.
– Ideally RSI while in ice water bath. Avoid succinylcholine as paralytic agent as large concern for rhabdomyolysis leading to acute kidney injury (AKI), hyperkalemia and death.
– In peri-code situation, presume hyperkalemia, give pushes of calcium chloride, and consider ampules of sodium bicarbonate. Increase perfusion by increasing cardiac output with large volume crystalloid infusions.
– Dantrolene administration: Expensive medication without clinical data to support its use in this setting. There are two formulations for dantrolene administration: Dantrium/Revonto which are the older formulation and Ryanodex. Both options require reconstitution with sterile water to give 2.5mg/kg of dantrolene. Dantrium (20mg/vial) requires much larger amounts of sterile water (750 mL for 250mg injection of dantrolene) to give the correct dose. Ryanodex (250mg/vial) was preferred for practical reasons as the time to administration was much shorter given that it only needs to be reconstituted with 5 mL of sterile water for injection.
CASE 5:
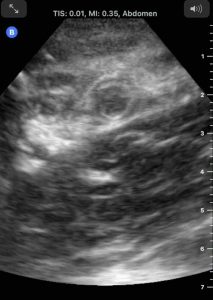
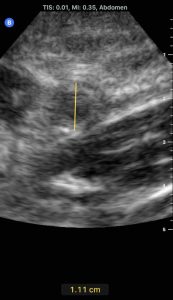
27M no significant PMH presented to a medical tent with diffuse abdominal pain for one day which then migrated to his right side with tenderness to palpation. Appendicitis was suspected and patient had a POCUS performed…
Teaching Points:
– POCUS appendix: place patient supine, place probe over point of maximal tenderness in RLQ, use graded compression until R psoas and iliac vessels (or appendix) identified. Appendix will appear as blind pouch in between or anterior to these structures. Normal appendix < 6mm and compressible.
– Acute appendicitis findings: outer diameter > 6-7mm, non-compressible, lack of peristalsis; some secondary findings: appendicolith/fecalith, free fluid, ring of fire (increased vascularity on color-flow doppler, thickened wall > 3mm, target sign, increased echogenicity of adjacent periappendiceal fat/omentum, enlarged mesenteric lymph nodes, thickening/hyperechogenicity of overlying peritoneum, thickened or dilated/hypoactive adjacent small bowel/apical cecal pole.
Other teaching points and pics:
– Ankle dislocations – First step is to assess the neurovascular status. Posterior dislocation – most common (associated with rupture of tibiofibular ligaments or lateral malleolus fracture). After pain control/anxiolytic, helps to bend at knee to relax gastrocnemius, have assistant pull counter traction, hold dorsum of midfoot with one hand and heel with other and pull longitudinally and anteriorly (if no assistant, have the patient hang leg over edge of stretcher).
Anterior – as above but dorsiflex foot to disengage talus, axial traction, push foot posteriorly while assistant pulls traction on tibia and pulls anteriorly. Lateral – plantarflex foot then apply traction with assistant holding counter traction.

– A male patient approximately 20 years old presented with AMS and dilated pupils and was found to be clonic. He was initially hyperthermic and was rapidly dunked in an ice-water bath. His glucose was normal. After approximately 7 minutes in the ice-water bath, he was no longer hyperthermic. Despite multiple doses of Versed (total 12mg IV), he remained clonic. The use of dissociation-dose ketamine was discussed to reverse his clonic muscle contractions and thus preventing further rhabdomyolysis but he was unable to maintain his airway and the patient was RSI’d and transported.
The patient was extubated the next morning neurologically intact and discharged. The patient was somehow brought back into festival by friends, and presented in the same condition the next day! This time ketamine (0.5 – 1 mg/kg IV) was used with resolution of his clonus and we were able to avoid intubating and transporting the patient for the second time in two days. In this scenario, ketamine was an effective treatment to dissociate patients with clonic, agitated episodes. The patient was observed to sobriety and after extensive counseling, discharged with advice to find better friends.
– Another treatment option for Status Epilepticus – Ketamine is an NMDA antagonist thereby blocking glutamate from binding to NMDA receptors. Glutamate is an excitatory neurotransmitter thus ketamine administration results in decreased CNS activity and is an effective treatment for status epilepticus. The dose recommended is: initial loading dose of 1.5 mg/kg IV push over 3 – 5 mins); max 150 mg. Repeat until seizures stop; max total load of 4.5 mg/kg. A ketamine infusion might be necessary at a dose of 1.2 mg/kg/hr; titrate to seizure suppression.
Perhaps the greatest lesson reinforced was one that is well established within our specialty. Whether in the emergency department or in austere environments, we as emergency physicians do not dictate our patients’ individual life choices or what will arrive to the ambulance bay or medical tent on any given shift. We found that good teamwork and understanding each provider’s skill and training level, knowledge of disaster preparedness principles with awareness of resources and limitations, and putting patients’ needs first regardless of their actions were paramount in providing sound medical care in this remote, austere environment.
As we reflect on our individual decisions to be on the front lines of healthcare, we are entrusted by patients to care for them despite any self-injurious behavior they impose on themselves. Much like in the emergency department, the initial rapport developed with each patient was paramount to provide competent care as it enabled us to communicate with each patient in an open and non-judgmental way.