A male in his mid 40’s presented with 20 minutes of chest pain in the middle of the night. He had no previous cardiac disease. After looking at his first ECG, you see there is sinus rhythm with left bundle branch block (LBBB).
This case, sent by one of our residency graduates who has learned all about STEMI in Left Bundle Branch Block (LBBB), demonstrates how you have to advocate for your patient. You have to be the expert. I talk to a lot of emergency physicians who have trouble convincing their interventionalist colleagues of various ECG findings. It is very important to establish a good relationship with your interventionalist colleagues, so that when difficult cases arise, the patient gets the care they need.
Case
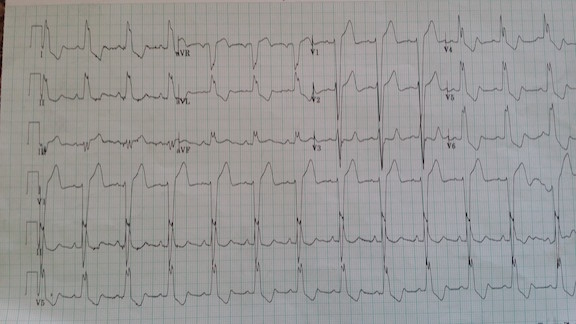
A male in his mid 40’s presented with 20 minutes of chest pain in the middle of the night. He had no previous cardiac disease. See figure 1 for his first ECG.
There is sinus rhythm with left bundle branch block (LBBB). [LBBB because the The QRS is wide (> 120 ms), there are wide upright R-waves in lateral leads I, aVL and V6, the “intrinsicoid deflection” (time from beginning of the QRS until its peak) is 50 milliseconds (50 ms)]. As with all LBBB, there is a small r-wave in V1-V3 and a deep S-wave.
Can you diagnose STEMI here? —Yes!
The diagnosis of STEMI in the presence of left bundle branch block has been problematic for years.
Until recently, the guidelines for management of Acute MI recommended cath lab activation for patients with chest pain and new LBBB. This was a nearly useless recommendation, as it turns out that only approximately 2-4% of patients who present to the ED with chest pain and new LBBB have acute coronary occlusion, and this is no different than patients who present with old LBBB [1]. Thus, the 2013 guidelines abandoned this recommendation, with a nod toward use of the Sgarbossa criteria, which are well known to be specific, but not sensitive [2]. There are many physicians, including cardiologists and interventionalists, who still believe that you cannot diagnose STEMI in the setting of left bundle branch block and who are unaware of the Sgarbossa criteria [2], as well as of the Smith-modified Sgarbossa criteria [1].
In fact, in normal conduction, ST elevation on the ECG is only about 70% sensitive for the diagnosis of coronary occlusion; in LBBB, the modified Sgarbossa criteria likely have a similar sensitivity. There are many reasons for the mistaken idea that MI cannot be diagnosed in the presence of LBBB and they go way back in history, but are beyond the scope of this article.
The diagnosis of STEMI in LBBB is dependent on the “Rule of Appropriate Discordance,” which means that, in normal LBBB (without MI), the ST segment (and usually T-wave) are in the opposite direction (discordant to) the majority of the QRS. “Concordance” (ST segment in the same direction as the QRS) is abnormal and indicates STEMI. Sgarbossa and others have found high specificity of an ST segment that is concordant to the QRS. For instance, in lateral leads there is always an upright R-wave and so, if the ST segment is elevated, as it may be in lateral STEMI, it is diagnostic of STEMI if there is just one lead with ≥ 1 mm of concordant STE. In LBBB, V1-V3 always have a predominant S-wave (QRS is predominantly negative) and therefore ST depression (STD) in V1-V3 is always concordant; ≥ 1 mm of STD in just one of these leads is diagnostic of STEMI (posterior STEMI, in fact). Finally, where Sgarbossa found 5 mm of discordant STE to be fairly specific for MI,* we found that an ST segment that is discordantly elevated out of proportion (≥ 25%) to the preceding S-wave was much more sensitive and accurate than a 5 mm absolute cutoff.
*[The full explanation of Sgarbossa’s point system is beyond our scope here; for our purposes, we will consider 5 mm of discordant ST elevation to be positive for the “unweighted” Sgarbossa rule.]
Because in LBBB, in leads V1-V3, the QRS is always predominantly negative (deep S-wave), the normal state of a patient with LBBB is ST Elevation in these right precordial leads. So how can you diagnose anterior STEMI in LBBB (unless there is proximal LAD occlusion producing a lateral MI with concordant STE)? Only if that STE is out of proportion.
Modified Sgarbossa Criteria [1]
≥ 1 lead with ≥1 mm of concordant ST elevation
≥ 1 lead of V1-V3 with ≥ 1 mm of concordant ST depression
≥ 1 lead anywhere with ≥ 1 mm STE and proportionally excessive discordant STE, as defined by ≥ 25% of the depth of the preceding S-wave.
Sgarbossa herself apparently likes this modification, as she and Cai incorporated it into their very nice algorithm [3].

Figure 2
See figure 2 for an ECG with only sinus tachycardia and LBBB; there is no evidence of coronary occlusion, as all ST-T complexes are discordant and appropriately proportional. There is no concordant STE. There is 5 mm of discordant STE in lead V2, but the S-wave is 40 mm, for a ratio of 5/40, or 0.125, which is a normal ratio. Thus, by the unweighted Sgarbossa criteria, it is anterior STEMI, but by the ratio rule, it is non-ischemic. This turned out to not be MI or acute coronary syndrome, as predicted by the rule.
Let’s go back to the case we started above. Look again at the ECG:
There is subtle concordant STE in lead aVF, almost 1 mm. There are about 2 mm of discordant STE in lead III. Since the S-wave is only 3 mm, this is proportionally excessively discordant ST elevation.
You should be very worried about STEMI here and, if you are reluctant to activate the cath lab, you should at the very least contact your cardiologist for an emergent formal ECHO, and obtain serial ECGs at least every 10-15 minutes to look for evolution.

Figure 3
Within minutes, the patient devolved into ventricular fibrillation. He was resuscitated. See figure 3 for the post-resuscitation ECG:
Now there is tachycardia, which can exaggerate discordant STE, but should never cause concordant STE, which is now clearly seen in leads III and aVF, with reciprocal proportionally excessive ST depression in aVL and aVR. Lead V3 has an inexplicable QRS with profound concordant STE. So this is clearly diagnostic of STEMI (There is also ST depression out of proportion: > 30% of the R-wave in leads V5 and V6) [1].
The cath lab was activated. When the interventionalist heard that the patient had LBBB, he was furious and stated that “you cannot diagnose STEMI in the presence of LBBB!” (He said this even though there was a cardiac arrest!) When he arrived and saw the ECG, he insisted that all ECG findings were due to post-resuscitation changes (comment: while arrest can result in similar findings, the first ECG already showed the findings in their more subtle form). He stated: “You inappropriately called in the cath team. The only STEMI by criteria is 2 mm ST Elevation in 2 consecutive leads with normal QRS and it is the cardiac arrest that created these ECG abnormalities.”
The emergency physician insisted that it was STEMI and instructed the interventionalist on the modified Sgarbossa criteria.
He did take the patient to the cath lab and found a 100% acute RCA occlusion. But he continued to insist that there are no ECG findings of STEMI in patients with LBBB except for new LBBB.
Learning point: You need to be the ECG expert and advocate for your patient. The emergency physician’s confidence in her diagnosis could have been undermined by the interventionalist. She could have doubted herself and relented. But she had learned about LBBB and the modified Sgarbossa criteria well enough to be confident. She was also aware that consultants are fallible, and have various holes in their knowledge base. So she was able to be persistent in advocating for the patient, and do so diplomatically, so that the interventionalist would not resist.
Imagine how resistant the interventionalist would have been if the patient had no cardiac arrest, but chest pain only.
REFERENCES
1. Smith SW, Dodd KW, Henry TD, Dvorak DM, Pearce LA. Diagnosis of ST Elevation Myocardial Infarction in the Presence of Left Bundle Branch Block using the ST Elevation to S-Wave Ratio in a Modified Sgarbossa Rule. Annals of Emergency Medicine 2012;60:766-76.
2. Sgarbossa EB, Pinski SL, Barbagelata A, Underwood DA, Gates KB, Topol EJ. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. N Engl J Med 1996;334:481-7.
3. Cai Q, Mehta N, Sgarbossa EB, et al. The left bundle-branch block puzzle in the 2013 ST-elevation myocardial infarction guideline: From falsely declaring emergency to denying reperfusion in a high-risk population. Are the Sgarbossa Criteria ready for prime time? Am Heart J 2013;166:409-13.









6 Comments
Convincing interventionalists to act has always been difficult, and near impossible at night. Now I have a new tool to sell them on STEMI in LBBB.
Imagine how difficult it is for a paramedic to try and convince the ED staff to activate the cath lab in these cases?
Regarding the 3rd ctiteria if we are to say that there is a more than 25% ST elevation in a negative QRS complex lead that if counted turned out to be less than 5mm.. Will i take it also consider it as a -ve sgarbossa?
Thanks
“There are about 2 mm of discordant STE in lead III.” In lead III I see a positive QRS with ST elevation (concordance). Was this a typo?
You may be looking at the post-resuscitation ECG, they were analyzing the first ECG at the title of the article.
Thank you for this case presentation. I am a paramedic and have used the Sgarbossa criteria or the modified version on a few occasions. Unfortunately there are some EM physicians who have been resistant to such presentation and insist on “No STEMI can be diagnosed with LBBB.”