You’re having a rough shift: The ED is out of metoclopramide and prochlorperazine, so you worry that you’ve been turning migraineurs into drug-seekers by treating them with promethazine and hydromorphone. You know that sodium bicarbonate is running low, so you hope that you don’t see a bad tricyclic overdose any time soon.
How to effectitvely treat alcohol withdrawal during nationwide shortages of benzodiazepines
You’re having a rough shift: The ED is out of metoclopramide and prochlorperazine, so you worry that you’ve been turning migraineurs into drug-seekers by treating them with promethazine and hydromorphone. You know that sodium bicarbonate is running low, so you hope that you don’t see a bad tricyclic overdose any time soon. And your friend from obstetrics is having trouble treating ectopic pregnancy without methotrexate, and she suggested that the two of you show up to the next Pharmacy and Therapeutics Committee meeting in handcuffs as an expression of your frustration. Hoping to put this out of your head you pick up the next chart. Chief complaint: Alcohol Withdrawal. “Great” you think, “and we’re supposed to be reserving IV alprazolam and midazolam for status epilepticus. I sure hope this guy can take POs”.
The patient is a 42-year-old male accompanied by his wife. He got a DUI on Thursday and, after a bender on Friday that spilled into Saturday morning, he quit drinking cold turkey about 48 hours ago. He reports nausea with intermittent vomiting. He feels anxious, but he denies any other complaints. On exam you notice a fine tremor and beads of sweat on his forehead. His heart rate jumps from the 90’s to the 110’s when you start talking to him, and his blood pressure is 156/98 although he denies a history of hypertension. The remainder of the H&P is normal, and you are satisfied that he has clear-cut alcohol withdrawal without complicating factors, so he should be able to go home with his wife if you can just get his symptoms under control. The vomiting makes oral meds unlikely to succeed, your nurses vociferously despise the CIWA protocol, and since it’s a typically busy Monday, you’d really like to get this patient dispositioned by the end of your shift in two hours. What are you going to do if you can’t use IV benzodiazepines for this patient? Just then, you remember one of your “old school” attendings from residency who used to sing the praises of phenobarbital for alcohol withdrawal. It’s not on shortage…yet. So you decide to give it a try.
Alcohol withdrawal (AW) is a common condition with significant morbidity and mortality. Parenteral benzodiazepines (BZDs) such as diazepam and lorazepam have commonly been considered first-line agents for moderate to severe AW. But, due to nationwide shortages of BZDs, EPs are now being required to limit our use of their injectable formulations. Since AW is not going to go away any time soon, now is a good time to consider our alternatives.
Baclofen, antiepileptics, dexmetomidine, propofol and barbiturates have all been studied as therapeutic options for AW, but only barbiturates have been consistently shown in comparison trials to be as efficacious as benzodiazepines when given parenterally for the treatment of alcohol withdrawal1,2,3. Due to their pharmacokinetics, BZDs require repeat dosing to prevent recurrence of withdrawal symptoms. In patients who are discharged this often necessitates prescriptions involving potentially confusing tapering dose regimens – a suboptimal plan in this population with dubitable compliance. In contrast, phenobarbital (PB) has a long half-life (50-140 hours) thereby avoiding the need for repeat dosing after achieving adequate symptom control4. In 1987, Young et al used IV PB to treat AW. In patients without alcohol or other sedatives present at the time of enrollment successful symptom control was achieved in 96% with a mean IVPB dose of 598 mg. 92% of patients were discharged and the investigators reported no readmissions. None of the subjects required admission for excessive sedation. In 2011, Hendey et al compared IVPB plus outpatient placebo to IV lorazepam plus outpatient chlordiazepoxide and found similar efficacy and safety between the two agents. In Hendey’s study the mean dose of PB was 509 mg with a discharge rate of 88%, and there was no significant difference in ED length of stay, hospitalization rate or 48-hour Clinical Institute Withdrawal Assessment (CIWA5) score between the LZ and the PB groups, although one patient treated with IVPB returned for seizure.
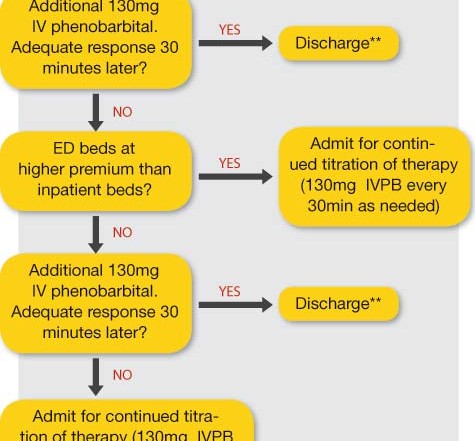
IV PB comes in 1 ml vials containing 130mg each. We have had good success with the following approach to adults who have moderate withdrawal symptoms and are suitable for discharge if symptoms can be controlled:
1) Give an initial IV PB dose of 260 mg IV (2 vials)
2) Reassess 30 minutes later. If the response is inadequate . . .
3) Give a repeat dose of 130mg
4) Reassess again in 30 minutes.
-If symptom control is achieved, the patient can be discharged without the need for a prescription.
-If the patient’s symptoms are not controlled, continue giving 130mg every 30 minutes while preparing for admission.
Considering that the aforementioned studies’ mean doses were over 500mg and they reported no admissions or return visits for oversedation, it is safe to consider a 3rd dose of IVPB for a total of 520mg prior to deciding whether to admit the patient. Your individual preference will depend on individual patient factors, such as preference and social situation, and whether your ED beds are at a higher premium than your inpatient beds or if your ED is experiencing significant boarding problems. The above approach is outlined in the flow chart. If your patient is in severe AW, then the dose of PB can be more aggressively titrated up until you have achieved an adequate response, similarly to how you would dose BZDs. As with BZDs (and perhaps more commonly), higher doses of PB may lead to hypotension and/or respiratory depression. Thus IVPB remains an excellent choice for the treatment of severe AW, but these patients typically require admission.
Because IV PB has an approximately five minute onset of action and will usually reach peak effect within 30 minutes, all of this can be done with only 90 minutes from institution of therapy to disposition decision. Additionally, because injectable phenobarbital comes in 1ml vials containing 130mg/ml, this regimen is easy on the nurses and does not require medication wasting (a good thing to avoid with our current rates of drug shortages).
After an initial dose of 260mg IV the patient had improved but was not yet ready for prime time. So you ordered another 130mg, and 30 minutes later he was calm but alert. His heart rate came down to 84 and his BP was 122/86. The tremors and diaphoresis had resolved, so you wrote his discharge order before signing out all the boarders to the next shift.
References
1. Hjermo I, et al. Dan Med Bull. Aug 2010;57(8):A4169.
2. Hendey GW, et al. Am J Emerg Med. 2011;29(4):382-385.
3. Young GP, et al. Ann Emerg Med. 1987;16(8):847-850.
4. Hvidberg EF, Dam M. Clin Pharmacokinetics 1976;1(3):161-188.
5. Sullivan JT, et al. Br J Addict. 1989;Nov:84(11):1353-7.