Follow these tips to be sure not to miss a big surprise.
You’re working an overnight shift in the emergency department with a new medical student. A 22-year-old female patient with abdominal pain appears on the tracking board and he eagerly signs up and leaves the work area to evaluate her. He returns after a few minutes and says “I can’t get very much history or do a physical exam because she is in too much pain. Can we give her some pain medication first?”
He tells you that the patient has right lower abdominal pain that woke her from sleep approximately 45 minutes ago. She is crying because her pain is so severe and he is worried she has appendicitis. By this time, the nurse has populated the vital signs: blood pressure 110/60, heart rate 98, temperature 37 °C, SpO2 97% on room air and respiratory rate 22.
You order some pain medication and go see the patient with the student. She appears to be quite uncomfortable, tearful and holding her lower abdomen. She says “I felt fine before I went to bed. I’ve never had this much pain before.” She denies trauma, vomiting, diarrhea, dysuria, back pain, dyspnea or fevers. Additionally, she reports her period started yesterday and denies abnormal discharge. On exam, heart sounds are regular, lungs are clear, abdomen is diffusely tender to palpation with guarding and she seems to have the most pain with palpation in the right lower quadrant.
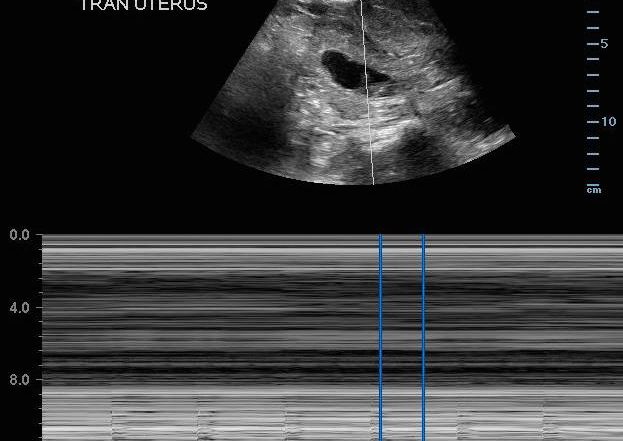
You pull the ultrasound machine in the room and have the medical student start scanning. He shows you the following:

He says, “I couldn’t find her appendix, but she’s pregnant! So we need to get an MRI to look at her appendix. And the fetus has a good heart rate.”
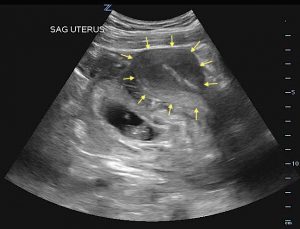
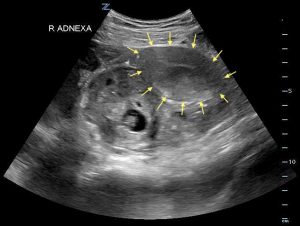
Realizing he made a classic error, you take the probe and scan the patient. You show him the images again.
You point out the uterus anterior to the gestational sac and fetus, and ask him again about his diagnosis. With a surprised look, he says “An ectopic pregnancy?” In agreement, you update the patient as to your findings and plans to call OB. She looks at you, shocked, and says, “But there is no way I can be pregnant!” You show her the picture again and assure her that she does indeed have an eight-week ectopic pregnancy causing her abdominal pain.
- Transabdominal, sagittal ultrasound showing gestational sac and fetus posterior to uterus (yellow arrows outline uterus).
- Transabdominal, transverse ultrasound showing gestational sac and fetus in right adnexa (yellow arrows outline uterus).
Your OB colleagues evaluate the patient and decide on operative management; she recovers well.
PEARLS/PITFALLS:
- Scan with enough depth to look for free fluid. Fluid typically collects first in the posterior cul-de-sac as this is the most dependent portion of the pelvis; you need to see the inferior-most aspect to assess for free fluid and clots. Occasionally, patients may have isolated fluid in their anterior cul-de-sac, particularly if they have a retroverted uterus.
- Don’t initially zoom in on the fetus; you can more easily miss an ectopic pregnancy. Look on transabdominal ultrasound for the relationship of the fetus, yolk sac, and gestational sac to the uterus and bladder. The bladder is immediately anterior to the uterus. An intrauterine pregnancy should appear in the fundus of the uterus, just behind the bladder. It is easy to get excited about finding a fetus and then not confirm that it’s within the uterus; be systematic in your ultrasound approach. Look in both sagittal and transverse planes and evaluate both adnexa. A transabdominal ultrasound should always be performed before a transvaginal ultrasound.

Normal intrauterine pregnancy. Gestational sac and fetal pole are seen in the uterus, directly posterior to bladder.
- If free fluid is found in the pelvis, look in the right upper quadrant. Fluid in Morison’s pouch in a suspected ectopic pregnancy is highly predictive for operative intervention (1). Free fluid should look like a dark, hypoechoic stripe between the liver and kidney or around the liver tip.

Ultrasound view of right upper quadrant. Free fluid is seen in Morison’s pouch between the liver and right kidney, visualized as a black hypoechoic stripe.
- Make sure you ask the patient about assisted reproduction! Risk of heterotopic pregnancy in a woman who conceived naturally is approximately 1 in 4,000 to 30,000. The risk in a woman using fertility treatments is as much as 1 in 100 (2). If used, the chances of a heterotopic pregnancy are significantly higher than in the general population, so look closely at both adnexa, even if an intrauterine pregnancy is found.
- Pay attention to the bladder. Perform a transabdominal scan with the patient’s bladder full. Have the patient empty their bladder just prior to a transvaginal ultrasound.
- A definitive intrauterine pregnancy is a gestational sac with a yolk sac or a fetal pole. A woman does not have an intrauterine pregnancy with a gestational sac alone or with a double decidual reaction. You must see a yolk sac or fetal pole within the gestational sac to diagnose a definitive intrauterine pregnancy. It is possible to have a pseudo-gestational sac within the uterus with an ectopic pregnancy.
- Ultrasound regardless of the serum hormone level! A serum beta-hCG level should not determine whether or not an ultrasound is performed to evaluate for a pregnancy. Ectopic pregnancies have abnormal development and can be present and rupture at levels far below the discriminatory thresholds (3).
- M-mode for heart rate. Use only M-mode to measure fetal heart rate in first trimester. Doppler should be reserved for second and third trimesters only. Doppler should be reserved for second and third trimesters only, due to concerns about heat transmitted to the first trimester fetus when obtaining fetal heart rate.
References:
- Moore C, Todd WM, et al. Free Fluid in Morison’s Pouch on Bedside Ultrasound Predicts Need for Operative Intervention in Suspected Ectopic Pregnancy. Academic Emergency Medicine. 2007;14(8):755-758.
- Tal J, Haddad S, Gordon N, et al. Heterotopic pregnancy after ovulation induction and assisted reproductive technologies: a literature review from 1971 to 1993. Fertil Steril. 1996;66(1):1-12.
- Kohn MA, Kerr K, Malkevich D, et al. Beta-human chorionic gonadotropin levels and the likelihood of ectopic pregnancy in emergency department patients with abdominal pain or vaginal bleeding. Acad Emerg Med. 2003;10(2):119-126.