You are working in a busy ED when a one-year-old presents with first time wheezing, rhinorrhea and fever. The child is tachypneic at 44 breaths/minute and has mild indrawing accompanying the diffuse wheezes. Oxygen saturations are normal (98%) on room-air. The child is tolerating breast feeds well and appears well hydrated. You make the clinical diagnosis of bronchiolitis.
The Setup:
You are working in a busy ED when a one-year-old presents with first time wheezing, rhinorrhea and fever. The child is tachypneic at 44 breaths/minute and has mild indrawing accompanying the diffuse wheezes. Oxygen saturations are normal (98%) on room-air. The child is tolerating breast feeds well and appears well hydrated. You make the clinical diagnosis of bronchiolitis. You hope to improve the child’s respiratory condition enough for a successful discharge home. Having a multitude of options to treat this child you devise a plan of action.
The Choices:
Your patient is experiencing bronchiolitis with mild features of respiratory distress. The best option for treatment of this child’s condition is:
- Nebulized albuterol (AKA salbutamol, Ventolin)
- Nebulized epinephrine
- Hypertonic saline
The Bottom Line:
When controlled for patient severity, three doses of nebulized albuterol are significantly better than a single dose of nebulized epinephrine for discharging pediatric patients with bronchiolitis.
Bronchiolitis is most common between the ages of two and six months, occurring exclusively in children younger than two years old. In the United States, bronchiolitis is the leading cause of hospitalization during the first year of life accounting for 21% of admissions costing $500 million annually. Bronchiolitis results from an acute lower respiratory tract inflammatory response to a (usually) viral infection that produces small airway obstruction manifest as tachypnea, chest retractions, wheezing, and hypoxia.
So how do I apply this new evidence to my patients?
When treating children with bronchiolitis inhaled salbutamol is a viable option and if effective in the ED can be prescribed as an outpatient.
One Cochrane systematic review found bronchodilators only produce a short-term benefit in infants with bronchiolitis. Another Cochrane review found that inhaled epinephrine may not be superior to inhaled salbutamol for bronchiolitis.
Use what works for your individual patient. The advantage of trying inhaled salbutamol for bronchiolitis is that if you show benefit for an individual patient you can prescribe salbutamol as an outpatient.
Caveats:
This is a well-performed randomized controlled, blinded study of two inhaled options for the treatment of bronchiolitis. There are a few confounding problems with this study:
Children in the salbutamol group were administered three doses where the children in the epinephrine group only received one dose followed by two treatments with nebulized saline.
A recent Cochrane systematic review found that hypertonic saline is an effective therapy for bronchiolitis management.
In most cases neither salbutamol or epinephrine is likely to be useful, minimizing the importance of any difference between the two.
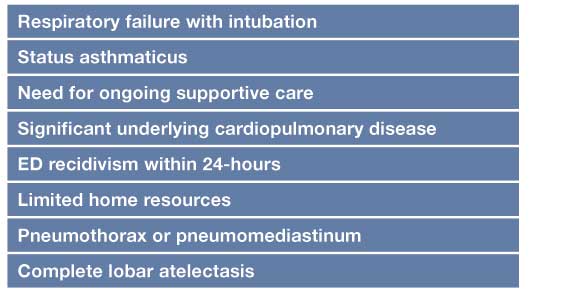
Bronchiolitis management is variable. Evidence-based bronchiolitis guidelines have been developed to standardize care. Although each case must be treated individually, general considerations for admission have been suggested (Table).

Case Outcome:
You try administering nebulized salbutamol with little effect. A dose of nebulized epinephrine has the same effect. The child is observed for three-hours during which time he continues to have normal saturations and feeds well. You explain to the parents why steroids are not being used and discharge the child with specific instructions to return to the ED if there are deteriorations in the child’s hydration, respiratory effort, activity level or mentation.
Anthony G. Crocco MD, FRCPC, is an emergency physician at the Alberta Children’s Hospital in Calgary, Canada.









1 Comment
This is a great article. I’ve read in many other places before that but
I did not get this type of effective and more useful text. It is really important now to
vary your anchors as this seems more natural to user.
This article helped me a lot to understand information.
Nebulizer