Handling the difficult detection of testicular torsion.
It’s around 2 a.m. on a Tuesday morning after a busy Monday evening in the emergency department. You’ve spent the majority of the evening so far putting out proverbial “fires” after coming on to cover the nocturnal shift at the local rural community hospital.
The waiting room has now been decompressed significantly with two patients remaining to be brought back. As you review the tracking board, you note an 11-year-old male with a chief complaint of vomiting and 48-year-old female with dyspnea. Both patients are listed as level 4 lower acuity, so you decide to start with the older patient who had the longer length of stay nearly three hours after initial presentation.
As you complete her history and physical, you feel a little anxiety about the pediatric patient awaiting an evaluation for his presenting illness. In your experience, pediatric vomiting in most cases is associated with gastroenteritis in addition to some other non-threatening differential diagnoses.
The initial impression as you walk into the room is an anxious patient in some discomfort. He is holding an emesis bag and looks tired. His father is at bedside and re-affirms an acute onset of intermittent abdominal pain with subsequent non-bloody, non-bilious emesis. While his pain is localized to the lower quadrant, physical examination of the abdomen is fairly benign. He is embarrassed to admit to you that he has had some occasional testicular pain as well.
Initial Examination
“Whoa! It’s really gotten much bigger,” asserted the patient’s father as he looks on during your exam of the patient’s scrotum. The patient said he noticed swelling “every now and then.” “He complained of some pain and bigger size down there a few weeks back, but I thought he was going through puberty,” the father explained.
As you continue your exam, you find that the asymmetry of the patient’s testicle is quite obvious. On palpation, the right testicle is high riding, firm and quite tender. You also notice that the scrotum is mildly erythematous and edematous. It transilluminates well and his cremasteric reflexes are absent.
As your priorities immediately change to manage this patient with suspected testicular torsion, you mobilize personnel to transfer the patient to the closest pediatric hospital nearly three hours away as your hospital does not have the resource to manage the patient’s condition. You treat the patient’s pain and consider ordering a formal ultrasonography.
Knowing the sonographer would have to be called in and that the resulting read can be predictably slow at night, you decide to confirm your suspicion with a bedside ultrasonography examination.
Findings
The machine is a little older, but it has capabilities to detect vessel flow with Doppler. You explain the exam to the patient’s father and proceed to bring the machine to the bedside along with warm gel. Using the linear probe, you first scan the unaffected, non-edematous and non-tender testicle to determine vessel flow and doppler. You note trace fluid collection around the testicle, which has a hyperechoic homogenous echotexture (Figure 1).

Longitudinal view of the left testicle. Note homogenous, hyperechoic echotexture.
Selecting the color feature, you immediately notice diffuse patchy red and blue pulsations indicating flow of the testicle. You then activate the Doppler and place the marker over one of the red pulsating echoes, which display a distinct waveform strip (Figure 2a).

Pulse-wave doppler of the left testicle with (a) arterial waveform and (b) venous waveform.
Attempting a similar feature on one of the non-pulsating echoes yields another different waveform you recall being venous flow (Figure 2b).

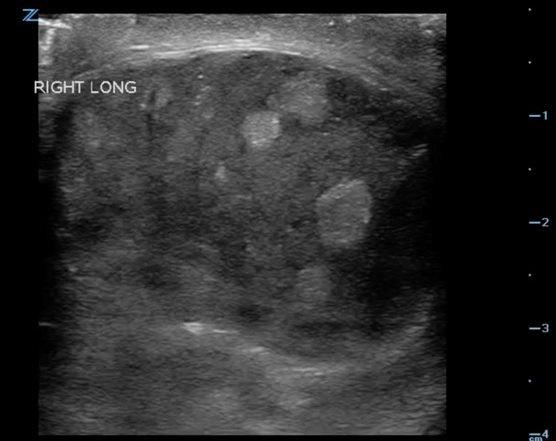
A similar evaluation of the affected testicle is heterogenic, hyper/hypoechoic and some fluid collection (Figure 3).

Longitudinal view of the right testicle. Note heterogenous, hypoechoic with areas of hyperechoic echotexture.
Scanning further, you note a lack of pulsating red and blue echoes. Your Doppler fails to give a consistent waveform. You attempt to increase the frequency holding the transducer ever so still, yet there is no pulsating or waveform activity (Figure 4).

Pulse-wave doppler of the right testicle with absence of flow
Admittance
If you were initially somewhat uncertain about your clinical exam, this confirms your suspicion. You discuss your finding with the father and medical team. You instruct the ED secretary to put out a page for the on-call pediatric urologist at the children’s hospital where you plan to transfer the patient.
The on-call urology resident calls back and before completing her salutation, you quickly state that “I am very concerned about an 11-year-old with a right testicular torsion.” After giving a brief history, you explain your exam findings and mention that the ultrasound was done at “bedside and was suggestive.”
She sounds a little surprised before saying “we would be happy to accept the patient, but would it be possible to confirm your findings with a formal ultrasound as you wait for transfer?” In response you explain that there’s no guarantee that the read will be confirmed in time as the transfer team has already arrived.
From the sound of her voice, you surmise that she is not completely convinced yet said that she will notify her attending immediately. Due to the distance and time sensitivity of the situation, you requested the patient to be flown. Additionally, you completed the transfer process by speaking directly with ED attending at the children’s hospital, informing them that the patient has not had any formal imaging.
Conclusion
While there is some level of confidence in your clinical and bedside skills, doubt and anxiety about transferring this patient without any formal imaging to confirm your bedside diagnosis begin to enter your mind. As the end of your shift, you personally called the children’s hospital ED to inquire about the patient.
As it turns out, both ED physicians and the on-call Urology team confirmed physical exam findings immediately on presentation and a formal ultrasound performed in the radiology department likewise confirmed your finding. The attending on the other end of the line reports that the patient was taken to the operating room within an hour of arriving to the ED, but there’s no word on whether the testicle was salvageable.
Teaching Points
- Testicular torsion is a urologic emergency which commonly present with acute onset testicular pain that may be intermittent, representing episodes of spontaneous de-torsion. Vomiting and abdominal may subsequently follow.
- The clinical evaluation of testicular torsion can be augmented by the use of POCUS ultrasound and may serve as a triage tool for rapid identification, allowing for mobilization of resources to facilitate medical and surgical management.
- Evaluation of acute testicular pain is time-sensitive and can be diagnosed clinically and by ultrasound, which is the modality of choice. Any delay in treatment increases the risk of testicular loss and infertility. POCUS can be a useful tool to augment clinical evaluation with a sensitivity and specificity approaching 100% and 90% respectively.
- On average, salvage rates are cited between 80 to 100% if surgery is performed in a timely fashion (within 5 to 6 hours on pain onset). Conversely, only 20% are salvaged if surgical intervention is performed within 12 to 24hours.
- POCUS findings are dependent on the duration of the torsion with venous flow being compromised before arterial blood flow. The result is often a progressively hypoechoic, edematous and painful testicle over time as infarction ensues. Vascular flow can be assessed using color or pulsed-wave Doppler, which is essential.
- A careful physical examination precedes sonographic evaluation of the testes making sure to identify the surrounding anatomical structures, cremasteric reflex, the vertical or horizontal lie of the testicle and the asymmetry of the contralateral testes.
- An ultrasound machine with a linear high-frequency transducer is optimal for best assessment and evaluation of the testes. The sonographer should proceed with the patient in a supine and comfortable position, and added support including towels and warm gel. Note that the best position for anxious young children may be on the parent’s lap.
- One should scan both testicles individually in the sagittal and transverse plane as well as simultaneously (side-by-side) for comparative assessment of size and echogenicity. It is vital to scan through the entire testicle beginning with the unaffected side if possible, to optimize assessment of the testicular anatomy and flow.
- Doppler with arterial (pulsatile) and venous (low and continuous) waveforms are essential in evaluation of testicular torsion for assessment of testicular perfusion. (Figure 2a, 2b). Additionally, perfusion may be difficult to detect in prepubertal boys who generally have smaller testicular vessels and lower blood-flow velocities that may lead to false-negative sonographic examination.
- The normal testes appear hyperechoic and homogenous with Doppler flow (both arterial and venous) when compared to a torsed testicle, which maybe hypoechoic with areas of hyperechoic echotexture and heterogenous without flow.
Pearls and Pitfalls
- POCUS testicular torsion assessment is an adjunct to the bedside physical examination. When used correctly, it serves to enhance rapid mobilization of resources for this time-sensitive urologic emergency.
- In the formal sonographic-limited setting, POCUS can be a great tool but should not delay or impede management of suspected testicular torsion. Remember that adequate pain control and supportive care while evaluating the presenting complaint often improves patient experience. Furthermore, gentle examination for patient comfort is important to success of the POCUS being performed.
- Recall that while the proper doppler flow and gain significantly improve the bedside exam, mistaking the extratesticular flow (which includes the epididymis) for intratesticular flow can lead to false-negative interpretation.
- Since early or partial torsion may show arterial without venous waveforms, interpretation of the POCUS exam can be misleading resulting in critically missed torsion. Be aware that arterial waveforms may be slightly diminished and may appear as venous waveforms due incomplete torsion. This maybe a subtle difference in distinguishing between the two waveforms as the arteries should always have flow even in diastole.
- As in our case subacute or chronic torsion can present with scrotal wall thickening and a reactive hydrocele (Figure 3). Additionally, enlargement of the testicle is seen as it becomes heterogenic and hypocheoic with areas of hyperechoic echotexture, primarily due to congestion, hemorrhage and infarction.
- When clinical diagnosis of testicular ultrasound is made by the examiner, early and immediate activation and consult of specialty care (Urology) for likely surgical intervention is critical to the time-sensitive nature of this diagnosis.
- The therapy for testicular torsion is surgical exploration, detorsion and fixation of both testis, with orchiectomy for nonviable testis. In the event of prolonged delay for management or if diagnosis is made prior to severe scrotal edema, the experienced physician can attempt a manual detorsion, rotating the testes outward toward the thigh (“opening the book”). Adequate analgesia and a doppler ultrasound is also a useful adjunct when considering this procedure.
- Current studies on POCUS for testicular torsion are limited to case reports and retrospective, however have shown encouraging success when utilized by the emergency physician with ultrasound experience, supporting a role for POCUS to evaluate patients presenting with acute scrotal pain.
References
- Doniger, SJ. Pediatric Emergency and Critical Care Ultrasound. 2013. Cambridge Medicine.
- Marin et al., 2016 Pediatric emergency medicine point-of-care ultrasound: summary of the evidence. Crit ultrasound.
- Fleisher and Ludwig. Textbook of pediatric emergency medicine. 2010. 6th Lippincott Williams and Wilkins. Chapter 57. 475.