How would you treat this bite victim?
A museum snake handler was bitten on the hand while transferring snakes to a display container. He is unsure which snake bit him.
Upon arrival to the emergency department, his vital signs are HR 97, BP 126/87, RR 35, SpO2 97% on room air, T 37.0°C. His exam is significant for rapid shallow breathing and the HEENT exam below. Lung sounds are normal. Extremity strength is normal throughout. Which of the following is the best next step in management?
A. Administer antivenom and admit for monitoring
B. Admit for IV IG therapy
C. Apply a splint to the extremity affected by the snakebite
D. Call the toxicologist to receive recommendations for the next steps
E. Discharge the patient with close follow-up
Correct answer:
A. Administer antivenom and admit for monitoring
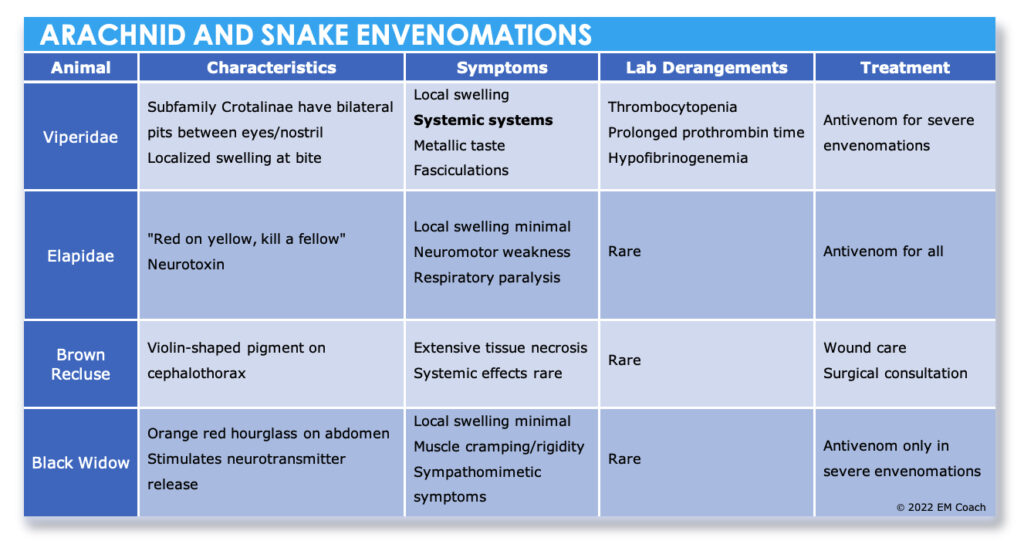
The patient was most likely bitten by a coral snake since he is experiencing signs of neuromuscular dysfunction. The picture shows bilateral ptosis, and the rapid shallow breathing is concerning for diaphragmatic weakness. Coral snake venom is a neurotoxin that can produce systemic neurological dysfunctions such as diplopia, ptosis, dysphagia, and possibly seizures. In this case, the patient is showing clear signs of envenomation and should be treated with antivenom and admitted for monitoring. Of note, the coral snake head is actually quite small, so the bites tend to be on small parts of extremities like fingers because the snakes cannot open their mouths wide enough to bite a large diameter extremity.
Incorrect answer choices:
Admitting the patient for IV IG therapy (Choice B) is inappropriate for snake bite treatment. IV IG would be appropriate therapy for a Myasthenia Gravis Crisis – which actually could present with similar clinical symptoms (absent the snake bite).
Applying a splint to the extremity involving the snakebite (Choice C) will help to prevent distribution of the venom; however, taking the time to apply a splint will delay the delivery of the antivenom. Splinting a limb affected by a snakebite is most useful when the patient needs to travel to get medical attention (e.g. in the prehospital setting).
The patient is already displaying signs of envenomation, which meets the criteria for antivenom, so calling the toxicologist to receive recommendations for the next steps (Choice D) would delay delivery of the antivenom. Remember as well that since this is the boards, calling a consultation to decide on a therapy is probably not the correct answer, even if you would probably do that in clinical practice. The examiners want to test YOUR knowledge, not that of the consultant.
Discharging the patient with close follow-up (Choice E) is inappropriate because the patient is showing signs of envenomation and needs to be admitted for monitoring and antivenom.
References:
Sheikh, S, Leffers, P. Emergency Department Management of North American Snake Envenomations. EB Medicine. September 1, 2018. Accessed June 15, 2022. https://www.ebmedicine.net/topics/toxicology-environmental/snake-bite-antivenom (full free access for residents)
Dart, RC, White, J. Chapter 212. Snakebite. In: Tintinalli JE, Stapczynski JS, Ma OJ, et al. <em>Tintinalli’s Emergency Medicine: A Comprehensive Study Guide</em>. 8th ed. New York: McGraw Hill Professional; 2016.