An 11-month-old otherwise-healthy male presents with his parents to the emergency department with a chief complaint of right elbow pain. He had experienced three days of fever and two days of tenderness at the right elbow prior to presentation.
The patient had been discharged from two different medical centers in the previous two days as his symptoms were presumed to be stemming from a viral upper respiratory infection. At the time of his current presentation, the patient is observed to be crawling without use of the right arm.
Physical exam revealed edema and warmth at the right elbow with no erythema. There were no abrasions or lacerations over the right elbow, and the patient has no known previous injury or trauma to the arm. Routine labs were notable for WBC at the upper limit of normal, with elevated neutrophil count and band percentage.
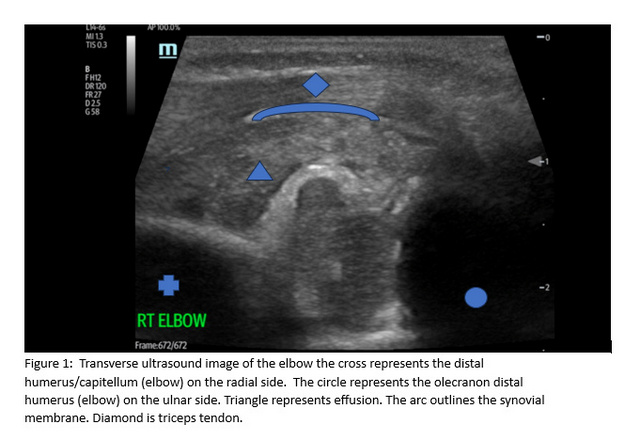
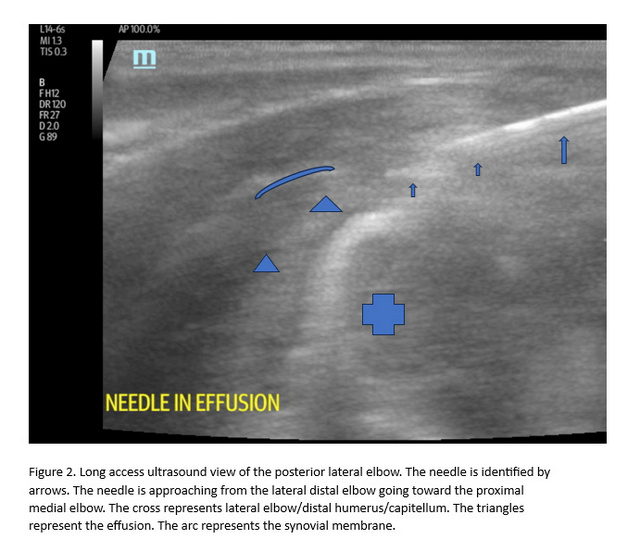
Given concern for underlying septic arthritis, point of care ultrasound was performed in the ED, which demonstrated joint effusion. Ultrasound-guided arthrocentesis was then performed in the ED, yielding <2 mL of bloody, purulent fluid from the joint space. (Please see figure 1 & 2). Blood cultures were collected and sent for analysis.
At this time, the patient was started on empiric antibiotic treatment and admitted to the hospital for emergent arthroscopic drainage and irrigation. During the operation, joint tissue was noted to be significantly edematous – weeping as it was incised. The surgical team encountered a large amount of thick, purplish cloudy pus in the joint. Necrosis of fascia and synovium necessitated fasciotomy and excision of the necrotic synovium.
After surgery, wound cultures showed growth of group A streptococcus and the patient was subsequently transitioned from empiric to organism-specific antibiotics. Although swift clinical improvement was expected status-post wound debridement and continuous antibiotic therapy, CRP levels remained elevated, and the patient remained febrile.
A post-operative MRI was ordered to evaluate for concomitant osteomyelitis, which has been shown to be associated with septic arthritis of the elbow joint, specifically [1].
Findings showed subperiosteal abscess of the distal radius, as well as diffuse fasciitis and myositis involving most of the forearm flexor and extensor muscle groups. Additionally, there was notable subperiosteal fluid and enhancement of the periosteum along distal radial shaft suggesting subperiosteal abscess.
Due to concerns of possible long-term complications stemming from incomplete wound debridement, a second washout was scheduled with the surgery team, which yielded additional purulent fluid. CRP began to downtrend after additional washout and continued antibiotic treatment, and patient was subsequently discharged on oral antibiotics.
At their six-month follow-up appointment, the patient was noted to be constantly running and playing at home, meeting all their developmental milestones. There were no abnormalities on physical exam and range of motion was full and intact in the affected elbow.
Infants with , or bacterial infection of a joint space, typically present with fever, increased irritability, poor feeding, and refusal to use the affected joint/limb [2]. These infections warrant particularly thorough evaluation in infants and neonates as physical exam and lab evidence may be subtle, more than one joint may be involved, and failure to treat may result in permanent damage [3,4].
Moreover, failure to initiate treatment promptly (within 3 days of symptom onset) is associated with increased risk of developing adverse sequelae [5]. Possible short-term complications include sepsis/shock, deep vein thrombosis, and septic pulmonary emboli, while long-term complications are comprised of potential joint laxity and/or dislocation, limited range of motion of the affected joint, limb-length discrepancies, and pathologic fracture [6,7].
However, in contrast to this case, most cases of septic arthritis in infants and neonates occur at the shoulder, hip, or knee, with infection of the elbow joint being significantly less common [1}. Further examination of case studies involving septic arthritis of the elbow in this population is needed to identify potential risk factors, differences in presentation, and possible adverse outcomes.
This case illustrates the utility of point of care ultrasound in the evaluation of possible septic joints. This patient had a relatively uncommon clinical presentation of septic arthritis, namely atypical joint location, and lack of obvious physical exam findings.
These factors contributed to a delay in initiation of treatment that could have potentially led to chronic adverse sequelae from the infection. In this instance, point of care ultrasound quickly and effectively identified the joint effusion, leading to prompt empiric treatment and avoidance of serious adverse outcomes.
References:
- Kaziz H, Triki MA, Mouelhi T, Bouattour K, Naouar N, Ben Ayeche ML. Septic elbow arthritis in children: Epidemiology and outcome. Arch Pediatr. 2019 Jan;26(1):38-43. doi: 10.1016/j.arcped.2018.11.001. Epub 2018 Dec 13. PMID: 30554847.
- Nade S. Septic arthritis. Best Pract Res Clin Rheumatol. 2003;17(2):183-200. doi:10.1016/s1521-6942(02)00106-7
- Dan M. Septic arthritis in young infants: clinical and microbiologic correlations and therapeutic implications. Rev Infect Dis. 1984;6(2):147-155. doi:10.1093/clinids/6.2.147
- Yagupsky P, Bar-Ziv Y, Howard CB, Dagan R. Epidemiology, etiology, and clinical features of septic arthritis in children younger than 24 months. Arch Pediatr Adolesc Med. 1995;149(5):537-540. doi:10.1001/archpedi.1995.02170180067010
- Welkon CJ, Long SS, Fisher MC, Alburger PD. Pyogenic arthritis in infants and children: a review of 95 cases. Pediatr Infect Dis. 1986;5(6):669-676. doi:10.1097/00006454-198611000-00014
- Arkader A, Brusalis C, Warner WC Jr, Conway JH, Noonan K. Update in Pediatric Musculoskeletal Infections: When It Is, When It Isn’t, and What to Do. J Am Acad Orthop Surg. 2016;24(9):e112-e121. doi:10.5435/JAAOS-D-15-00714
- Nade S. Septic arthritis. Best Pract Res Clin Rheumatol. 2003;17(2):183-200. doi:10.1016/s1521-6942(02)00106-7