Fractures of the metacarpals are among the most common orthopedic injuries seen by emergency physicians. Combined with phalangeal fractures, they account for ten percent of all fractures, and some studies estimate 20% of all fractures seen in the emergency department. Most injuries occur between the age of 11 and 45. A study in 1980 estimated that these fractures accounted for 90 million days of restricted work and 16 million days of lost work during the year studied [1,2]. At first glance these injuries seem straightforward, but as we will see, the complexity of hand anatomy and injury patterns demand detailed attention. Though highly specific, each fracture pattern and location may mandate variable treatment options. Failure to recognize some of the unique injury patterns can result in permanent disability.
As with all orthopedic injuries, a basic understanding of practical anatomy is critical. The hand is arguably the most mechanically complex orthopedic structure in the body. It’s not a coincidence that Hand Surgeons undergo five years of orthopedic or plastic surgery training followed by an additional one or two years of Hand Fellowship before mastering the assessment and treatment of these injuries.
The complexity of anatomy reflects the functional demands of the hand. Disability resulting from hand injuries can have life changing implications. A patient’s age, hobbies, vocation, and activity level are major determinants of how much functional disability can be tolerated. This can be highly variable from one patient to the next. More so then with any other orthopedic injury, an accurate assessment of these components of lifestyle is critical in determining treatment. The varying demands of activity, age, and vocation necessitate broad variability in treatment. A fracture pattern in one patient may warrant operative intervention while the exact same pattern in an other is treated with closed reduction and splinting, depending on their functional requirements. To add to the confusion, each hand surgeon will have a different threshold for what he or she believes can and cannot be tolerated.
As emergency physicians we sometimes minimize fractures of the metacarpals. What differentiates exceptional ED physicians is an in depth understanding of the varying determinants of treatment, along with the ability to communicate expectations and potential outcomes to patients.
Mechanism
Crush injuries, drop mechanisms and direct impact are the most common causes of metacarpal fractures. Punching injuries are unquestionably the most frequent mechanism of direct impact. Machine injuries typically have remarkable soft tissue damage and underlying fractures of the metacarpals are not uncommon.
Anatomy and Deforming Forces
It would be an exercise in futility to attempt a review all hand anatomy so I will focus on practical anatomy as it applies to treatment, healing, or potential disability.
The Interosseous muscles are the primary deforming force in metacarpal fractures. There are four dorsal and three palmar interosseous muscles. Remember PAD and DAB? (Palmar Adduct and Dorsal Abduct). Both, however, will flex at the MCP and extend at the IP joint. Because the muscles flex at the MCP, they are the primary deforming force in metacarpal fractures displacing the distal fragment toward the palmar side. An awareness of what forces you may be working against is extremely helpful when attempting reduction.
Clinical Evaluation
Tendon function should be assessed by evaluating abduction and adduction (Interossei), extension of the digits (common extensor tendon), and flexion at the MCP and DIP (Flexor Digitorum Superficialis and Profundus respectively).
The thumb should be tested independently with focus on the flexors and extensors at the IP and MCP joints. Extensor Pollicis Longus is tested by extension at the IP and Extensor Pollicis Brevis by extension at the proximal phalanx and metacarpal. The same joints are tested for Flexor Pollicis Longus and Flexor Pollicis Brevis with respective opposing actions. Opponens Pollicis should also be tested by opposing the thumb to the fifth finger and testing resistance.
 Exam Pearl
Exam Pearl
A functional evaluation of the hand is important when assessing metacarpal injuries. Put simply, this is an assessment of how the hand can perform basic functions such as opposition pinch and, most importantly, grip. This provides perhaps the most reliable information regarding what deformity or angulation can or cannot be tolerated. If the patient closes their hand and there is obvious overlap of grip and “loss of normal cascade” either closed or open reduction is required.
Cascade is essentially the normal alignment of fingers in a partial position of grip when allowed to completely rest with no applied flexion or extension. Normal cascade typically demonstrates a slight progression of resting flexion from the second to the fifth digit.
I find this functional assessment of grip and cascade the most valuable assessment in “Boxers Fractures” at the neck of the fifth metacarpal. Some radiographically will appear grossly deformed but have minimal to no affect on grip or cascade. Others with seemingly little angulation will grossly affect grip and cascade and accordingly I know reduction or surgery will be required.
Open Fractures
Open fractures of the metacarpals are not treated in the same manner as open long bone fractures. They can be classified by a number of formal systems but the most common (Swanson) is also simple and distinguishes them into two categories. This system is what I use when talking to my hand consultants and I like it because it’s easy, intuitive, and predictive of clinical outcomes.
- Type One: Clean, no significant contamination
- Type Two: Dirty, grossly contaminated
Including phalangeal fractures the incidence of infection for type one injuries is roughly 1.5% and for type two it is 15%. One to 2% is tolerated by most hand surgeons but 15% is not. Emergency physicians often feel as though the hand consultants are inappropriately minimizing open hand fractures by not taking them emergently to the OR for wash out. These data suggest that this is not necessary for Type One open fractures. Simultaneously when recognizing a grossly contaminated Type Two open fracture, an understanding of the classification and associated risk may help direct a sleepy consultant in the middle of the night [4,5,6].
“Fight bites” deserve their own discussion. These human “bites” that are usually the result of punching someone in the teeth are typically curve-linear and overlie the MCP. Fight Bites require antibiotic coverage even if they’re not showing evidence of infection. These injuries also require aggressive ED irrigation (2-3L). Obvious exudative drainage, an open MCP joint, or delayed presentation with evidence of infection requires surgical debridement and wash-out with admission for IV anti-biotics.
Controversies in Treatment
Interestingly, a ten year review published in 2010 demonstrated no increase in infection for immediate surgical fixation. Under normal circumstances an orthopedist would rarely put hardware in a contaminated open wound. It is one of the reasons external fixators are used. In open hand fractures this does not appear to be a problem. Patients who underwent acute surgical stabilization had no increased risk of infection associated with open fractures [7].
Metacarpal Fractures
Diaphysial (shaft) fractures
Fractures of the second through fifth metacarpal shaft are often the easiest to treat. As with most fractures, rotational deformity is not well tolerated. This is because rotation dramatically affects the alignment or “cascade” of the fingers as they close into a grip. Rotation creates mal-alignment in the cascade such that one digit is overlapping the other. Fortunately rotational deformity is rare in diaphyseal fractures.
The degree of dorsal angulation that can be tolerated varies among digits. Second and third metacarpals tolerate ten degrees of dorsal angulation while fourth and fifth metacarpals can tolerate up to twenty degrees. Operative intervention is indicated when reduction fails to achieve alignment within these parameters. Often this is due to interposed soft tissue. Surgery can involve percutaneous pinning with closed reduction (CRIF) or open reduction and internal fixation (ORIF).
Metacarpal Neck Fractures
These fractures are commonly seen in punching injuries and often need reduction. There is a tendency for ED doctors to minimize the need for reduction which can necessitate otherwise avoidable corrective surgery. Because we do not see these patients in follow up we are often unaware of the outcome.
The fourth and fifth metacarpals tolerate a great deal more angulation (30-40 degrees) than the second and third (10 degrees). These fractures typically displace with volar angulation.
The typical reduction technique is quite easy. One finger is placed on the shaft of the metacarpal, not extending beyond the fracture site, with the injured finger parallel to the floor. The MCP is bent at 90 degrees (pointing at the floor) and the phalanges are held in the other hand. Simultaneously the metacarpal is pushed down while an upward axial load is applied to the phalanges. See Figure A [8,9].

Treatment Controversies
Fifth metacarpal neck fractures – commonly referred to as “Boxer’s Fractures” – can tolerate a surprising degree of angulation. Some authors have suggested that up to 70 degrees can be tolerated so long as grip and cascade are not affected and there is no associated rotational deformity. Not all surgeons will agree on this extreme degree of accepted deformity but suffice it to say that functional assessment is equally if not more important than radiographic
assessment.
Metacarpal Base Fractures
The force and mechanism required to fracture the base of the second through fifth metacarpals is quite unique. When these fractures are seen, physicians should have a high suspicion for carpo-metacarpal dislocations as well as independent carpal instability or fracture. Many of these injuries will require surgery. Most are radiographically subtle but can be seen on a true lateral. The physician, however, must have sufficient index of suspicion to look for these associated injury patterns in the presence of metacarpal base fractures.
Intra-Articular Fractures
A good rule of thumb is that intra-articular fractures throughout the body have a high likelihood of requiring surgical fixation. The articular surface is a perfectly smooth surface accommodating millions of repetitive movements. Even the slightest displacement results in an irregularity that disrupts articulation and at minimum causes some degree of traumatic arthritis. Marked disruption of the articular surface can lead to functional disability. While not all intra-articular fractures require surgery, the ED physician should have a very high level of suspicion when any intra-articular displacement is seen. Recognizing intra-articular involvement is key when communicating with the consultant and also valuable when discussing expectations with the
patient.
Treatment Pearl
Most authors agree that 1mm of visible articular step-off or a fragment involving more then 25% of the articular surface warrant operative intervention in a high functioning active individual [8,9].
Thumb
The thumb metacarpal deserves special attention. Most fractures of the metacarpal shaft are stable and can be easily reduced. ED physicians should have a low threshold to reduce these with minimal accepted residual mal-alignment. Any intra-articular fracture involving the carpo-metacarpal joint with a fragment large enough for fixation warrants a hand consultation.
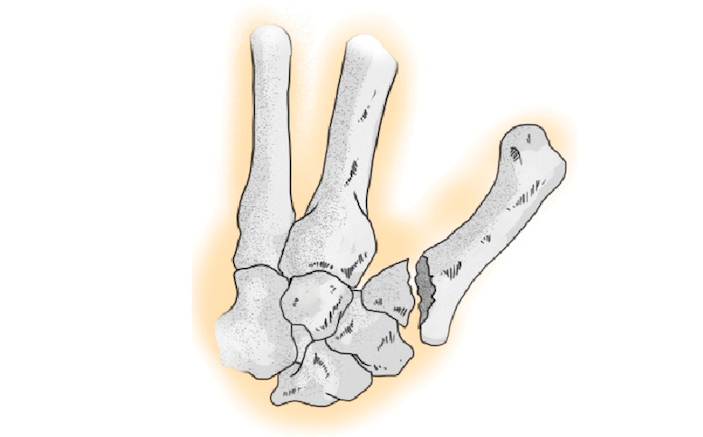
Fractures at the base of the thumb are unique because of their ligamentous insertion. Bennet Fractures (Figure B) are oblique intra-articular fractures at the base of the thumb in which ligamentous insertion holds the fracture fragment while the metacarpal itself displaces. These often require surgical fixation.

Carpo-Metacarpal Dislocations and Subluxations
Thumb CMC dislocations are unique in that injuries often result from lateral forces secondary to torque on a gripped object. These lateral forces can sublux or dislocate the CMC joint. The joint will frequently reduce spontaneously immediately after the injury, but the patient is left with persistent ligamentous injury. This is what occurs in “Game Keepers Thumb”. The ulnar collateral ligament is torn resulting in instability of the CMC joint. This is tested by assessing ulnar and radial stability at the CMC joint. Rarely, the torn ulnar collateral ligament interposes into the joint space, or falls dorsally, preventing adequate opposition of the torn ends of the ligament. In this scenario, known as a “Stenner’s Lesion”, the ulnar collateral ligament cannot heal and the patient develops persistent instability requiring surgical repair.
Controversies in Treatment
Although dislocations often seem straightforward in the emergency room, the timing of immobilization and limits on early range of motion are highly variable and by no means universally agreed upon. It’s my opinion that early range of motion under the close care of occupational therapy is critical for functional recovery however understanding which injuries are stable enough to tolerate early range of motion is critical. Many Hand Surgeons are extremely conservative in their length of immobilization. A study of 100 metacarpal fractures assessed outcomes comparing functional casting which allowed for wrist and phalangeal range of motion with traditional casting which incorporated why wrist and fingers. The results demonstrated significantly improved outcomes when the wrist and fingers were not incorporated in immobilization, and need for delayed surgical intervention are highly variable. Open fixation was invented with the sole purpose of allowing early range of motion – we often forget as emergency physicians that most of the disability following any orthopedic injury relates to post injury range of motion. Therefore the timing of allowed range of motion in recovery is critical. Early fixation allows for immediate range of motion. Occupational therapy for what may appear to be a minor injury is critical in restoring functional capacity [8,9,10].
Conclusion
The hand is a very difficult topic to discuss in review. There are countless injury patterns, each of which may mandate a unique treatment plan. The topics covered are limited to the metacarpals. Independent dedicated discussion is warranted for injuries to the carpal bones as well as the Phalanges. A basic understanding of anatomy and deforming forces is hugely valuable when attempting reduction.
REFERENCES
- Wolfe, Scott W., et al. Green’s Operative Hand Surgery: Expert Consult: Online and Print. Elsevier Health Sciences, 2010.
- Kelsey, Jennifer L. Upper extremity disorders: a survey of their frequency and cost in the United States. Mosby, 1980.
- Van Onselen, E. B. H., et al. “Prevalence and distribution of hand fractures.” Journal of Hand Surgery (British and European Volume) 28.5 (2003): 491-495.
- Swanson, Todd V., Robert M. Szabo, and Daniel D. Anderson. “Open hand fractures: prognosis and classification.” The Journal of hand surgery 16.1 (1991): 101-107.
- McLain, Robert F., Curtis Steyers, and Michael Stoddard. “Infections in open fractures of the hand.” The Journal of hand surgery 16.1 (1991): 108-112.
- Swanson, Todd V., Robert M. Szabo, and Daniel D. Anderson. “Open hand fractures: prognosis and classification.” The Journal of hand surgery 16.1 (1991): 101-107.
- Bannasch, Holger, et al. “Ten Years Stable Internal Fixation of Metacarpal and Phalangeal Hand Fractures—Risk Factor and Outcome Analysis Show No Increase of Complications in the Treatment of Open Compared With Closed Fractures.” Journal of Trauma and Acute Care Surgery 68.3 (2010): 624-628.
- Konradsen, Lars, Poul T. Nielsen, and Elisabeth Albrecht-Beste. “Functional treatment of metacarpal fractures: 100 randomized cases with or without fixation.” Acta Orthopaedica 61.6 (1990): 531-534.
- Egol, Kenneth A., Kenneth J. Koval, and Joseph David Zuckerman. Handbook of fractures. Lippincott Williams & Wilkins, 2010.
- Rockwood and Green’s fractures in adults. Philadelphia: Lippincott Williams & Wilkins, 2006.









4 Comments
A couple errors/typos in this article:
The flexor digitorum superficialis tendon (FDS) is responsible for flexion at the proximal interphalangeal (PIP) joint and NOT the MCP as stated in the article.
Also, “gamekeeper’s thumb” is NOT an injury of the carpo-metacarpal (CMC) joint. “Gamekeeper’s thumb” is a disruption f the ulnar collateral ligament at the thumb’s metacarpo-phalangeal (MCP) joint.
Otherwise, a nice summary.
An EP who attempts reduction in the ED is then bound to an orthopedist’s standard of reduction. I’ve been instructed by more than a few orthopedists to splint in place (unless there is neurovascular compromise, skin tenting, dislocation, etc) and have them follow up in the morning (or Monday).
Thanks for the corrections MPIUS. Accurate on both accounts. Please continue keeping me on my toes!
Appreciate your input Chris. As you know this is highly variable from one institution to the next as is much of Emergency Medicine. At one of the institutions I’ve worked ED physicians performed all of the reductions and orthopedics is involved only if unsuccessful. IN the others we were expected to at least attempt reduction. This was not only the preference of the orthopedists but also a policy generated from the orthopedic committee. I do disagree on the point that we should avoid procedures because we may be held to a different standard. To me, this is to imply that we should not due any procedure, unless acutely life threatening. There are countless procedures performed in the ED that may be performed more meticulously in the hands of a specialist, but that does not mitigate our role in treatment. Otherwise we as physicians are reduced to triage nurses. Emergency medicine was founded on our willingness to move into the territory of our specialists. If however the ED physician is not competent in performing the procedure, then they should not perform the procedure regardless of weather it is expected or asked by the orthopedist. I respect your opinion and some of my colleagues share it.
Obviously, the two most critical factors are communication with the orthopedists and patient care. If the orthopedists or hand surgeons prefer to do the reductions, we should be happy to let them. Personally I find it rare that patients obtain follow up within 24 hours. Once outside 48hrs they are committed to surgery and the window for reductions lost. As an orthopedic resident we rarely had the time to perform these in a clinic of 30-50 patients and they just got bounced back to the ED. I’ve also found that when patients are uninsured, or in the not uncommon situation in which the orthopedist contracts with limited insurance companies, the patient is unable to obtain follow up without a few hundred dollars upfront. Injustice as it may be it is a reality and I end up seeing them back in the ED four days later.
Again, I appreciate your comments and more importantly, I appreciate you taking the time to read my article!