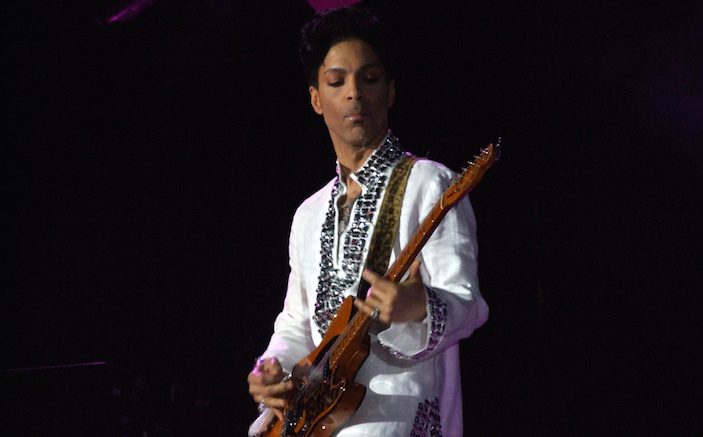
Prince’s recent death from a self-administered dose of Fentanyl could inflame anti-opioid sentiments to the point that legitimate uses are barred.
The recent death of Prince from a self-administered dose of Fentanyl could further inflame extreme measures attempting to limit or ban opioid prescriptions. However, focusing on the problems of opioid abuse in one segment of the population, without assessing the benefits of legitimate opioid need for the rest of the population, throws the balance from over-use to under-use.
Yes, we physicians have bought into the opioid hype: advertising by pharmaceutical companies, achieving a fabulous Press-Ganey satisfaction score, prescribing opioids to silence a patient’s complaints or to save time and avoid conversation about alternative remedies. It doesn’t help that our culture puts such a high value on immediate gratification and freedom from all maladies.
As far as EM practice goes, we need to improve our strategies and resources for patients who pop into the ED for acute exacerbations of chronic pain, or continuing difficulties with chronic pain. How many of us have provided referrals to physical therapy for chronic neck and back pain? Have we tried topical agents? Topical NSAIDS have less than a 1% systemic absorption and can be effective, as can lidocaine patches (available over the counter as 4% lidocaine) or topical rubefacients which contain salicylates. How about local lidocaine/steroid injections for conditions like painful trochanteric or shoulder bursitis or SI joint arthritis? Injection techniques (which used to be done in the ED, at least early in my career) have fallen out of favor but need new consideration. Since adjuvant analgesics (cyclics, SNRIs, SSRIs, GABA analogs, anticonvulsants) require time and dosage adjustments to be effective, most are best prescribed and managed by the primary care provider.
All that said, let’s not throw out the baby with the bathwater. A number of acute painful conditions are still appropriate for control with opioids: pain from malignancy, sickle cell anemia, trauma, severe orthopedic injuries, post-operative states, renal colic – just to name a few. And such acute problems often require more than 10 pills of oxycodone to get patients over the hump.
It’s a modern paradox that around the globe we prohibit pain relief for acute, severely painful conditions. Go visit Mexico and develop a kidney stone—you will not receive an opioid in the ED. In labor? Sorry, no pain meds allowed. Broken leg? Live with it; it’ll heal. In another off-balance gesture, the WHO attempted to severely restrict the use of ketamine in low-resourced countries due to concern for abuse. They’ve since retracted that restriction [1]. Ketamine can be a great ED alternative to opioids for acute pain—and emergency physicians need to be advocates for its use, and for its proper dosing.
So our attention has finally been caught: but rather than backing off from treating pain, we need to encourage our societies to help us develop and effectively use the best strategies for controlling pain.
REFERENCE
- International Anesthesia Research Society (IARS). “Restricting ketamine would have ‘dire consequences’ for surgery in low-resource countries, anesthesiologists warn.” ScienceDaily. ScienceDaily, 8 February 2016. <www.sciencedaily.com/releases/2016/02/160208140721.htm>.
- Photo by Scott Penner