Suturing isn’t the best option for the majority of digit injuries.
Finger injuries are one of the most common injuries seen in emergency departments, with estimates exceeding 5 million visits in the U.S. annually. Millions more are seen in urgent care centers and private offices. About 80-90% involves soft tissue injury that may require wound closure, with suturing remaining the most popular method used by providers. However, the literature just doesn’t support suturing uncomplicated finger lacerations less than 2 cm, which make up better than 80% of the finger injuries we see.
Most providers are familiar with Quinn’s 2002 UC San Francisco study that concluded that there is “no clinical benefit” to suturing uncomplicated finger lacerations less than 2 cm. Not only is there no benefit, when compared to merely washing out and bandaging these wounds, suturing takes 15 minutes longer, is more painful, increases the infection rate and requires a costly and inconvenient follow up visit for suture removal. Essentially, the UCSF study recommended we stop suturing these lacerations.
The study left us in a bit of a pickle. Millions of small, uncomplicated finger lacs are sutured each year, despite evidence that shows no benefit and a lot of downside – wasted provider time, decreased ED throughput, unnecessary painful injections, increased cost of care, and millions of unnecessary follow up visits each year for suture removal. However, merely washing out the wound and putting a bandage on it really isn’t a great option; patients expect more, especially after waiting several hours. As emergency medicine providers, our training is to fix things, do procedures, provide definitive care — we just needed a reasonable alternative.
How about Topical Skin Adhesives on Digits?
There are many advantages of using topical skin adhesives (TSAs) for small lacerations. TSAs are faster and easier than sutures to use. They can be applied without injections, reducing pain and anxiety while eliminating the risk of a needle stick. They also have a lower cost than using sutures and a laceration tray, a lower infection rate and eliminate follow up visits for suture removal.
While these advantages quickly led TSAs to be widely accepted and commonly used on other parts of the body, many providers find them challenging to use on digits. Lacerated fingers can bleed profusely, making it difficult to apply a topical skin adhesive or wound strip. The wound edges are often irregular and difficult to approximate, increasing the likelihood of inadvertently applying the TSA into the wound, which increases the chance of infection and wound dehiscence. Providers also express concerns that even when properly applied, the TSA will come off prematurely due to friction, frequent washing or high wound tension.
Topical Laceration Closure™ (TLC™) methods now allow the effective use of TSAs on digits. The T-RING is a one size fits all digit tourniquet that immediately provides the required bloodless field without the risks associated with the other commonly used digit tourniquets.
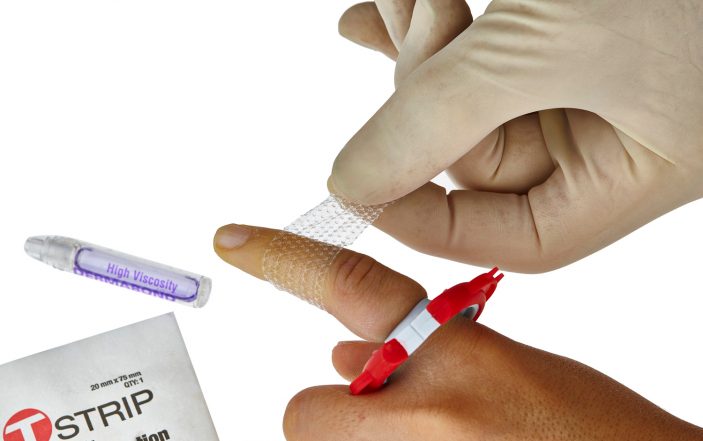
The T-STRIP is a porous, transparent, adhesive mesh that allows ideal wound approximation, while also reducing wound tension.

TLC™ materials
Once in place, a topical skin adhesive (TSA) is applied over, through and around the edges of the T-STRIP to seal the wound. The T-STRIP and skin adhesive provide a clear wound seal that allows ideal wound visualization throughout the healing process, while providing a protective barrier to dirt and infection.
The combination T-STRIP and TSA simply falls off in approximately 10-12 days, without need for a follow up visit for removal. Finally, the newer TSAs (octyl cyanoacrylates) are stronger and more flexible than first generation TSAs; making them more suitable for closing digit lacerations.

Before TLC™
Literature: TLC™ on Digits
Initial studies using the TLC™ methods noted above to treat simple finger lacerations have demonstrated their effectiveness. Most finger lacerations can be treated with topical anesthesia, avoiding the use of a laceration tray and a painful digital block. Treatment time using TLC™ is approximately one-third that of suturing similar lacerations, significantly reducing visit time and improving ED throughput. Initial results show that the T-STRIP and topical skin adhesive remain on a digit an average of 11.2 days, and had a complication rate (wound dehiscence, infection, recurrent bleeding) of 5.0%, compared to 9.4% for similar lacerations that were sutured.

After TLC™
Treating fingertip avulsions with topical laceration closure methods is a game changer- no laceration tray, no painful injections, no cautery or Surgicel. Simply apply the T-RING and topical lidocaine, rinse with tap water, apply a couple layers of a topical skin adhesive and you’re finished in less than five minutes. The TSA seals the bleeding vessels to immediately stop bleeding, while providing a protective “cap” that decreases pain and provides an ideal healing environment — keeping moisture in, and dirt and bacteria out. The cap simply sloughs off in about 10-12 days. There’s no need for painful soaks, dressing changes or routine follow up visits. And since you’ve closed the wound with a TSA, you can now be reimbursed for a wound closure.

Summary
Topical laceration closure methods offer many advantages when treating finger lacerations and fingertip avulsions. With the development of the TLC™ system, there is no good argument for suturing small, uncomplicated finger lacerations. Sutures provide no clinical benefit, they increase pain and infection, and once you place that first suture, a follow up visit is required. With greater than 80% of the 10-15 million finger injuries seen in U.S. EDs, urgent care clinics and private offices each year meeting the criteria for topical laceration closure, there is great potential for us to provide better, more efficient and more cost-effective care.





6 Comments
Talk about a conflict of interest. Please disclose the authors affiliation in the beginning.
This article is a thinly veiled advertisement by the inventor masquerading as a legitimate article. The editors who allowed this article to be printed were incompetent and/or nepotistic. You have now set a precedent that those interested in promoting their inventions can do so free of charge in in your publication.
I’m confused… Is this an advertisement for the trade marked TLC product?
I am offended that I spent 5 minutes in between patients, reading this “article” . The conflict is so obvious that it renders the entire article suspect. Your publication and editors should be ashamed.
Umm…Can you say BIASED? This “article” reeks of it, reading more like a medical magazine advert than a legitimate and professional journal type publication void of any ulterior motives. I kind of feel duped and misled. Any and all author disclosures should be clearly stated at the very START of the article; not the end.
I am a patient that had an over 1.5in laceration to my thumb on Thanksgiving night (cut by washing a lead crystal bowl). NP at the ER gave me 2 nerve blocks on either side of my thumb which is now PERMANENT and travels up my forearm, to put in 4 stitches and I have the same pain in that thumb over the laceration (even though the scar is almost invisible) that I had when I cut it (feels like between a cut or a burning sensation). I dont believe there is anything I can do about it at this point, however, I type for a living & cannot stand to even brush up against my thumb or forearm without pain. THIS type of treatment looks like it wouldve been wonderful for my laceration (when I had the sutures removed, I was told it was very deep).