Endovascular therapy should be considered in patients with persistent symptoms despite medical therapy
A 40-year-old female presented to the emergency department as a category two trauma activation 1.5 hours after she fell off her horse and was stomped over her chest.
The patient was evaluated at an outside hospital prior to transfer and was diagnosed with fractures of 2nd-7th left ribs and hypotension with a blood pressure of 80/50, which improved after administration of 1 L IVF. On arrival to our emergency department, the patient endorsed diffuse chest pain and shortness of breath, despite administration of 175 mcg of fentanyl at the outside hospital.
The primary survey was notable for an intact airway with no trachea deviation, but bilateral JVD was present. Bilateral diminished breath sounds were noted with saturations of 100% on a non-rebreather facemask. Palpable pulses were present in all extremities with an initial BP of 74/54, HR 80, and a respiratory rate of 12. Her GCS was 14 with no focal neurologic deficits.
The patient received 1 L of normal saline for initial treatment of her hypotension with two units of pRBCs ordered. The secondary survey was notable for midline C spine pain on palpation, and a diffusely tender chest wall with ecchymosis bilaterally over the anterior chest wall. The patient remained hypotensive despite fluids and active blood transfusion.
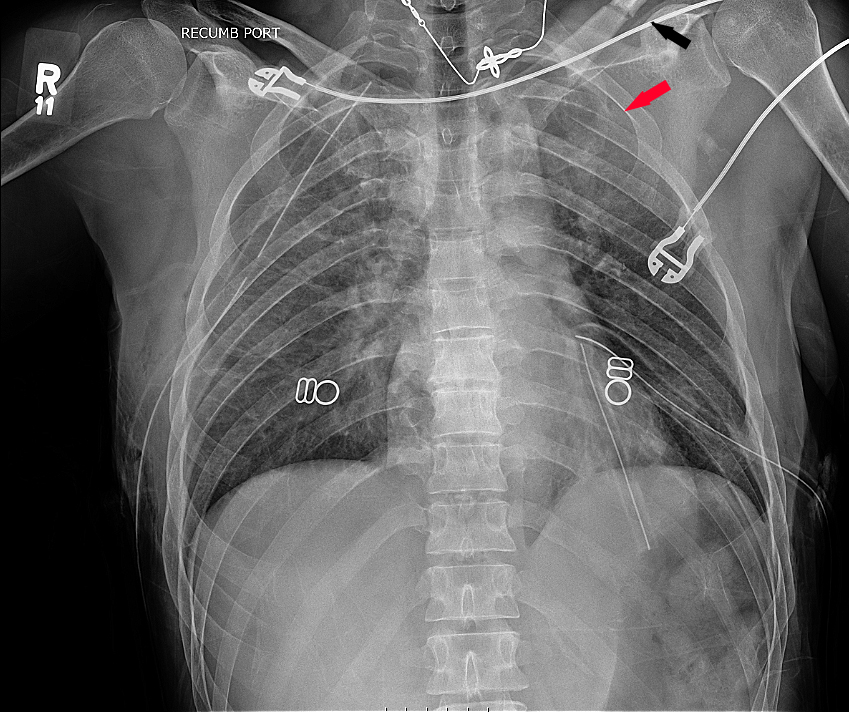
An E-FAST exam demonstrated no free fluid in the abdomen, no pericardial effusion, but bilateral pneumothoracies with a hemothorax on the right. Bilateral chest tubes were placed with return of air and 200cc’s of blood on the right and air on the left. A CXR after placement of bilateral chest tubes demonstrated a left clavicle and 3rd rib fracture (Figure 1, arrows).
The patient’s blood pressure improved to 122/52 and she was taken to CT scanner.
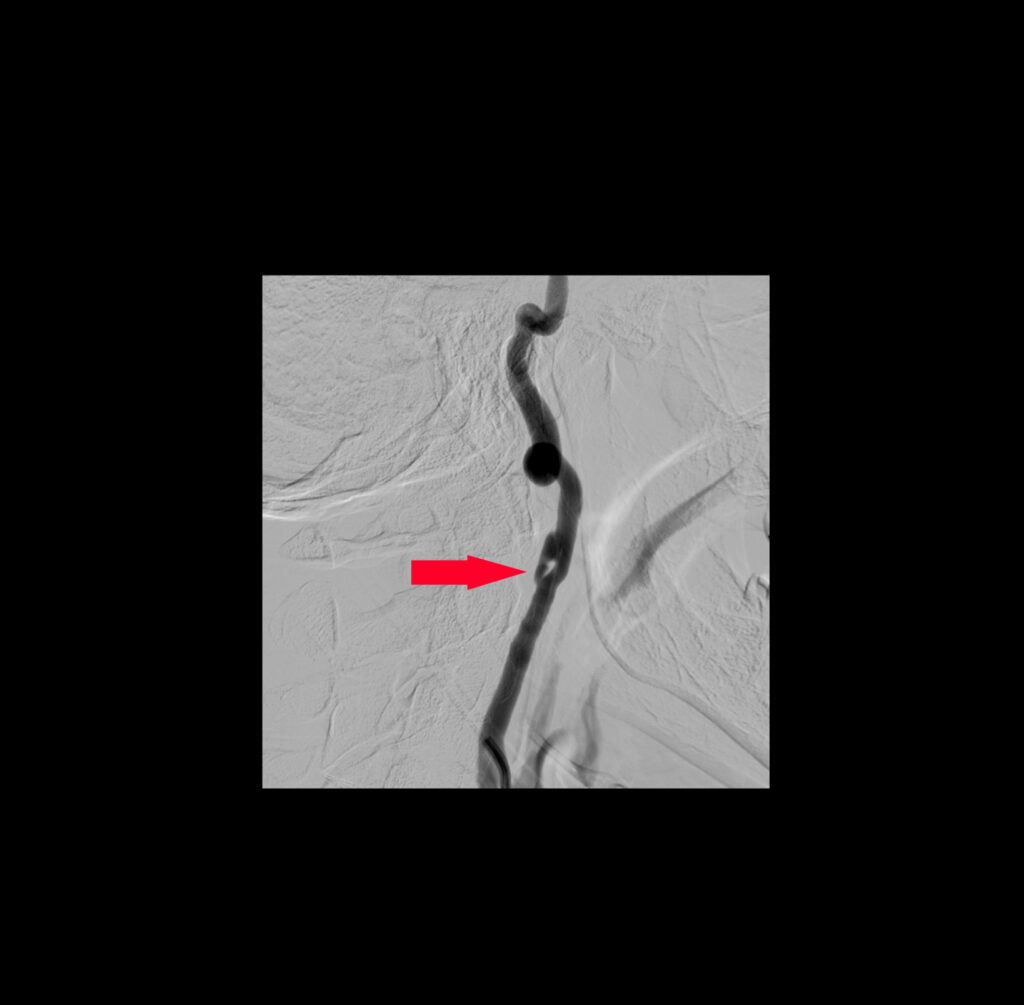
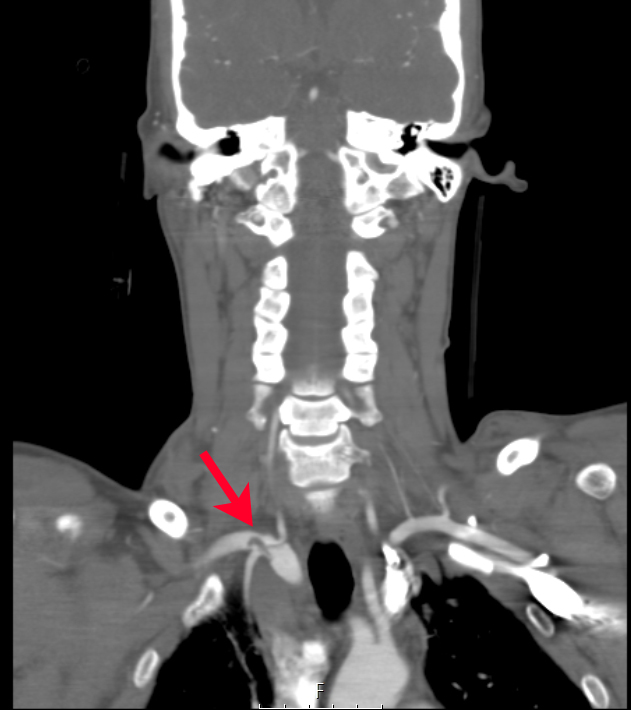
CTA of the neck and chest revealed multiple traumatic dissections including the left common carotid artery, the right internal carotid artery (figure 2a) at the level of C2, and the right subclavian artery (figure 2b). Additionally, fractures of the left 2-7th ribs, and the manubrium, were noted on her CT imaging.
Her laboratory studies were notable only for a leukocytosis at 25, no anemia with a hemoglobin of 12.1, a lactate of 2.3, and no coagulopathy. The patient was admitted to the trauma ICU for further management of her multiple traumatic vessel dissections, fractures, and bilateral pneumothoracies.
She was started on a heparin drip for treatment of her multiple dissections. The patient eventually had stent placements in the right carotid artery (figure 3a) and right subclavian artery (figure 3b) in addition to ORIF of her rib fractures with bilateral video-assisted thoracoscopic surgeries.
The patient was discharged in stable condition after seven days on dual antiplatelet therapy after stent placement. At her one month follow up visit, the patient had no complications.
Discussion
Traumatic carotid artery dissection shares multiple properties in therapy and pathophysiology with spontaneous vessel dissection. However, there are significant differences that must be considered when caring for these patients. Blunt carotid injury is noted in up to 2.6% of blunt traumatic injuries with cerebrovascular accident rates as high as 60% and mortality approaching 40%. Most carotid dissections are spontaneous with 4% of these dissections being traumatic in nature.[1]
Traumatic carotid dissections usually occur with direct blows to the neck or extreme flexion/extension of the neck. The most common presentations of a traumatic carotid dissection are embolic stroke, Horner’s syndrome, and cranial nerve palsy with variable time presentation from immediately after injury to months later.[1]
This presents a challenge to making the diagnosis as patients may have no symptoms suggestive of a traumatic carotid dissection on initial presentation. If a significant TBI has occurred, the patient’s brain injury may obscure findings of traumatic carotid dissection on physical exam. Criteria exist to assist in diagnosing blunt cerebrovascular injury including the Denver Group Criteria, Memphis Criteria, and Kerwin Criteria.[1]
These criteria emphasize consideration of the mechanism of trauma and specific injuries to the head and neck that should raise suspicion for BCVI. Ultrasound, CTA and MRA are all diagnostic tools, which can be used for the diagnosis of traumatic carotid dissection. MRA provides a high level of detail with cerebral vascular visualization but can lead to delay in diagnosis and may not be practical in an unstable patient or always be available. Ultrasound provides imaging of the neck vessels however, it cannot visualize the intracranial vasculature. CTA provides the most utility in general given its wide spread emergency availability with additional visualization of cerebral vasculature.[1]
The sensitivity and specificity of CTA for blunt cerebrovascular injury is noted to be 80% and 97% respectively.[2] The treatment of TCAD is centered around the prevention of thromboembolic events with anticoagulation or antiplatelet therapy initiated as early as possible.[1]
Early anticoagulation can present a challenge when there are concomitant traumatic injuries placing a patient at risk for hemorrhage. Risk for hemorrhage must be considered prior to initiation of anticoagulation in the ED. These patients require multidisciplinary management on a case-by-case basis.
Endovascular therapy should be considered in patients with persistent symptoms despite medical therapy, multi vessel involvement leading to hypoperfusion, expanding pseudoaneurysm, or contraindication to anticoagulation.[1] Patient’s with endovascular therapy will require appropriate antiplatelet therapy to prevent stent thrombosis for durations ranging from three months to indefinite depending on stent material and comorbidities.[1]
This patient was discharged in stable condition, ambulating without difficulty after seven days on dual antiplatelet therapy after stent placement. At her 1 month follow up visit the patient had no complications.
References
- Galyfos G, Filis K, Sigala F, Sianou A. Traumatic Carotid Artery Dissection: A Different Entity without Specific Guidelines. Vasc Specialist Int. 2016;32(1):1-5. doi:10.5758/vsi.2016.32.1.1 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4816018/ accessed 3/1/22
- Campbell D, Hoffman J. A Review of Blunt Cerebrovascular Injuries. EMRA Critical Care. 2019 February 5. https://www.emra.org/emresident/article/blunt-cerebrovascular-injury/ accessed 3/1/22